Every year, more than 130,000 people in the U.S. die from lung cancer. That’s more than colon, breast, and prostate cancer combined. And yet, most cases are still caught too late-when treatment options are limited and survival rates drop below 6%. But here’s the truth: if you’re a smoker or former smoker, there’s a real chance to catch it early, and if you do, your odds of living five years or longer jump to nearly 60%. The tools are here. The science is clear. The question is: are you getting screened?
Who Should Be Screened? It’s Not Just Who You Think
The old rule was simple: if you smoked a pack a day for 30 years and were over 55, you qualified. That’s outdated. In 2023, the American Cancer Society changed the game. Now, if you’re between 50 and 80, and you’ve smoked at least 20 pack-years-whether you still smoke or quit 20 years ago-you should be getting screened annually. A pack-year? That’s one pack a day for one year. Or two packs a day for ten years. Or half a pack a day for 40 years. It adds up faster than you think.
The U.S. Preventive Services Task Force still uses the 15-year quit cutoff, but that’s the problem. A 2022 study in JAMA Oncology found people who quit 15 to 30 years ago still had 2.5 times the risk of lung cancer compared to people who never smoked. That’s not a small risk. That’s a silent timer still ticking. The ACS got it right: if you smoked enough to be at risk, you’re still at risk-even if you haven’t touched a cigarette in a decade.
How Screening Actually Works: LDCT Explained
The only proven way to catch lung cancer early is a low-dose CT scan, or LDCT. It’s not a chest X-ray. It’s not a regular CT. It uses 70-80% less radiation than a standard scan, and it takes less than 10 seconds. You lie on a table, breathe in, hold it, and that’s it. No needles. No fasting. No prep.
But here’s what no one tells you: most positive results are false alarms. In the National Lung Screening Trial, 96.4% of people who got a positive scan didn’t have cancer. That’s why follow-up is critical. A small nodule might be scar tissue. Or inflammation. Or a benign growth. But if it grows over time? That’s when you act. That’s why screening must be done at an accredited center-where radiologists know how to read these scans and when to call for a biopsy, a repeat scan, or just watchful waiting.
And yes, AI is helping. In January 2023, the FDA approved LungQ by Riverain Technologies-the first AI software designed to flag lung nodules. It cuts down unnecessary follow-ups by 22%. That means less anxiety, fewer invasive tests, and more accurate tracking.
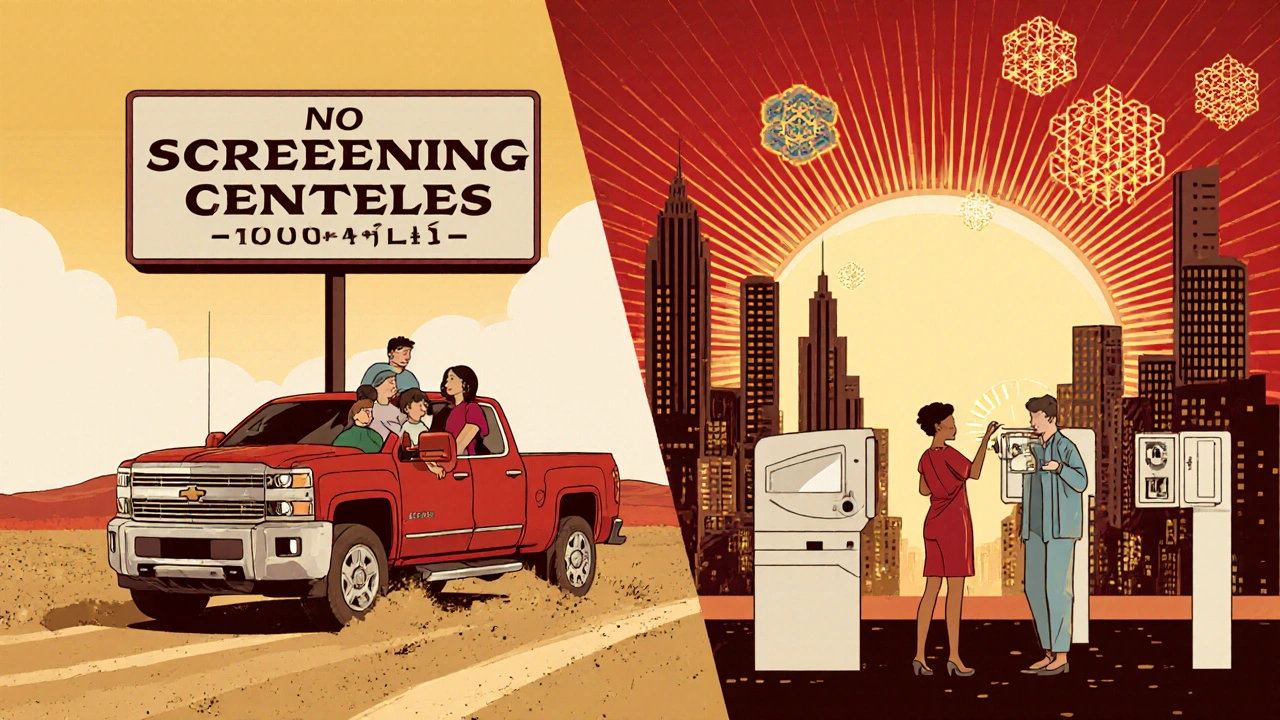
Why So Few People Are Getting Screened
Here’s the shocking part: only about 5.7% of eligible smokers in the U.S. are getting screened. That’s 2.6 million out of 45.5 million people who qualify. Why?
- Most primary care doctors don’t bring it up. A 2022 AMA survey found 42% of them didn’t even know the updated guidelines.
- Insurance coverage is messy. Medicare covers it for ages 50-77 with 20+ pack-years. But some private insurers still demand 30 pack-years and won’t cover anyone who quit more than 15 years ago.
- Access is uneven. Rural areas have 67% fewer screening centers than cities. If you live in a small town, you might need to drive 100 miles just to get a scan.
- Stigma still lingers. Many former smokers feel guilty. They think, “I brought this on myself,” so they avoid the doctor. But screening isn’t about blame-it’s about survival.
One solution? Electronic health record alerts. A 2021 study in JAMA Internal Medicine showed that when doctors got automatic prompts in their system, screening rates jumped by 32%. Patient navigators-people who help schedule appointments, explain results, and answer questions-boost adherence by 27%. These aren’t fancy tech fixes. They’re simple, human systems that work.
Targeted Therapy: When Early Detection Meets Precision Medicine
Screening doesn’t just find cancer early. It finds cancer that can be treated with precision.
Before 2020, surgery was the only option for early-stage lung cancer. Now, if your tumor has a specific genetic mutation-like EGFR, ALK, or ROS1-you can take a pill instead of going through months of chemo. Osimertinib, approved in 2020 for stage IB-IIIA non-small cell lung cancer, cuts the risk of recurrence by 83% after surgery, according to the ADAURA trial. That’s not a small improvement. That’s life-changing.
Here’s the connection: early-stage tumors caught by screening are far more likely to have these mutations than late-stage ones. The International Association for the Study of Lung Cancer predicts that by 2025, 70% of screen-detected cancers will have actionable targets. That means if you’re caught early, you’re not just surviving-you’re getting a treatment that’s gentle, effective, and tailored to your biology.
And it’s getting smarter. Liquid biopsies-blood tests that detect tumor DNA-are now being tested in trials like NCT04541082. The goal? To spot cancer signals in your blood before a tumor even shows up on a CT scan. Imagine screening with a simple blood draw, then confirming with a low-dose CT only if needed. That’s the future, and it’s already in motion.

The Big Picture: What Needs to Change
Screening saves lives. But only if it’s done right-and done often enough.
Right now, Black patients are 35% less likely to be screened than white patients. Rural residents face 42% fewer facilities. People with Medicaid or no insurance are often left out. These aren’t just statistics. These are people who could be alive today.
What’s needed isn’t just better technology. It’s better systems:
- Insurance companies must update their rules to match the ACS 2023 guidelines-no arbitrary quit-time limits.
- Hospitals must integrate smoking cessation into screening programs. Seventy percent of current smokers who get screened say they want to quit-but only 30% get help.
- Primary care providers need training, reminders, and support to talk about screening without shame.
- Community outreach must reach neighborhoods that have been ignored.
The goal isn’t just to find cancer early. It’s to stop it before it spreads. To turn a death sentence into a manageable condition. To make sure that if you smoked, you’re not just surviving-you’re living well.
What You Can Do Right Now
If you’re 50 or older and have smoked 20 pack-years or more:
- Ask your doctor: “Am I eligible for lung cancer screening?” Don’t wait for them to bring it up.
- If they say no, ask why. Check if they’re using outdated guidelines.
- Find an ACR-accredited screening center near you. The American College of Radiology has a public directory.
- If you still smoke, ask for help quitting. Screening isn’t a license to keep smoking-it’s a wake-up call.
- Get screened every year. No exceptions. Even if your last scan was clear.
One scan won’t save you. But 10 scans over 10 years? That could mean you’re here to see your grandchildren grow up.
What is a pack-year and how do I calculate mine?
A pack-year is the number of packs of cigarettes you’ve smoked per day multiplied by the number of years you smoked. For example, if you smoked one pack a day for 20 years, that’s 20 pack-years. If you smoked two packs a day for 10 years, that’s also 20 pack-years. Half a pack a day for 40 years? Still 20 pack-years. You don’t have to be a heavy smoker to be at risk.
Is lung cancer screening covered by insurance?
Medicare covers annual low-dose CT scans for people aged 50-77 with a 20+ pack-year history who currently smoke or quit within the last 15 years. Most private insurers follow this too, but some still use older rules requiring 30 pack-years or only covering people up to age 80. Always check with your insurer and ask for the specific guideline they use.
What if I quit smoking 20 years ago-do I still need screening?
Yes. Research shows former smokers remain at high risk for lung cancer for decades after quitting. The American Cancer Society’s 2023 guidelines removed the 15-year quit limit because studies found people who quit 15-30 years ago still had 2.5 times the risk of lung cancer compared to never-smokers. If you have a 20+ pack-year history, you should still be screened.
Can I get screened if I’ve never smoked?
Standard screening guidelines focus on smokers and former smokers because they make up 80-90% of cases. But non-smokers can still get lung cancer-especially due to radon, air pollution, or genetics. Right now, screening isn’t recommended for non-smokers unless they have a strong family history or a genetic condition like Li-Fraumeni syndrome. Research is ongoing to expand eligibility based on other risk factors.
What happens if my scan shows a nodule?
Most nodules are not cancer. Your doctor will compare your scan to previous ones (if any) and may recommend a follow-up scan in 3-6 months to see if it’s growing. If it grows or looks suspicious, you may need a biopsy. Only about 3.6% of people with positive screens end up with cancer. The key is not to panic-but to follow up.
Are there risks to getting screened every year?
The radiation from a low-dose CT is very low-less than a standard mammogram. The bigger risk is false positives, which can lead to unnecessary biopsies or anxiety. But the benefit of catching cancer early far outweighs these risks for people who qualify. If you have serious health problems that would prevent you from having surgery or treatment, screening may not be right for you. Talk to your doctor about your overall health before starting.

Just got my first LDCT last month after my doc finally brought it up. Turned out clean but I’m gonna keep doing it yearly. Scary how easy it is to ignore this until it’s too late.
My dad quit smoking 22 years ago but still got screened last year. Doc said even though he’s clean, his pack-years still count. Glad the guidelines changed. He’s alive today because of it.
I work in primary care, and I can confirm-most of us didn’t even know the guidelines updated until last year. We’re still using the old 30-pack-year cutoff because our EHR hasn’t been updated. It’s not laziness, it’s systemic neglect. Someone needs to push the IT departments.
I used to think if I quit, I was off the hook. Then I read that study about 15-30 years post-quit still having 2.5x the risk. I got screened last fall. Found a 4mm nodule. Watched it for 6 months. Still there. No growth. No panic. Just peace of mind. This isn’t about guilt-it’s about responsibility.
Let me tell you something real. I was a smoker for 28 years. Quit 12 years ago. My wife begged me to get screened. I told her I was fine. Then I got the call. Nodule. Biopsy. Stage IA. No chemo. Just surgery. And now I’m on osimertinib because my tumor had EGFR. I’m alive because I listened. I’m not a hero. I’m just someone who didn’t ignore the warning. If you’re reading this and you’ve smoked-you owe it to your family to get checked. Not tomorrow. Today.
Why are we even talking about this? In India we don’t have this luxury. My cousin died of lung cancer last year and they didn’t even have a CT scanner in his town. You guys complain about 5.7% screening rates? We have 0.3%. Stop acting like this is some universal problem-it’s a rich country luxury.
Interesting how the article ignores that LDCT scans cause more harm than good due to false positives. The NNT to save one life is over 300. That’s not efficient. And why are we pushing screening on people who are still smoking? It enables denial.
Why are we giving free scans to people who made bad choices? I worked 40 years, paid taxes, never smoked. Now I’m paying for smokers to get screened? This is socialism for bad habits. If you want to live longer, don’t light up in the first place.
Just read your comment, Joe. I get where you’re coming from. But my dad’s a Vietnam vet. He smoked because he was trying to cope with PTSD. He didn’t have access to therapy. He had cigarettes. Now he’s getting a second chance. Isn’t that worth it?
My uncle got screened last year, found cancer, had surgery, now he’s back to golfing. I told my mom to get checked too. She said she’s too old. I said, ‘You’re 62. You’re not too old to live.’ She went. Scan was clear. She’s still mad at me for pushing her. But I don’t care. She’s alive.