Pancreatic Cancer Staging Guide
Select a stage below to learn about its characteristics, treatment approach, and survival statistics.
Stage I
Localized cancer
Stage II
Locally advanced
Stage III
Regional spread
Stage IV
Distant metastasis
Stage I: Localized Cancer
Characteristics
- Cancer is confined to the pancreas
- Tumor is ≤ 2 cm in size
- No lymph node involvement
- No distant metastasis
Treatment Approach
Surgery with curative intent is typically possible. The Whipple procedure or distal pancreatectomy may be performed.
Survival Rate
Patients with Stage I pancreatic cancer have the best prognosis among all stages. Early detection and surgical removal offer the highest chance of long-term survival.
Staging Process
Accurate staging requires imaging studies (CT, MRI, EUS) and tumor marker analysis (CA 19-9). This information guides treatment decisions and helps predict outcomes.
Key Takeaways
- Pancreatic cancer is staged I‑IV using the TNM system, which guides treatment decisions.
- Early stages (I‑II) often allow surgery with curative intent; later stages focus on control and palliation.
- Imaging (CT, MRI, EUS) and tumor markers (CA 19‑9) are essential for accurate staging.
- Survival drops sharply from stage I (~25%5‑year) to stage IV (<3%5‑year).
- Multidisciplinary care-surgery, chemotherapy, radiation, and supportive services-improves outcomes at every stage.
What "Staging" Means in Pancreatic Cancer
When doctors talk about the pancreatic cancer is a malignant growth that starts in the pancreas, an organ tucked behind the stomach responsible for producing digestive enzymes and insulin. It’s one of the toughest cancers to catch early because early tumors cause few visible signs. Staging is the process of measuring how far the disease has spread. The most widely used method is the TNM classification, which looks at:
- T (Tumor): Size of the primary tumor and whether it invades nearby structures.
- N (Nodes): Involvement of regional lymph nodes.
- M (Metastasis): Presence of cancer in distant organs such as the liver or lungs.
Combining these three letters produces stages I through IV. Understanding each stage helps patients know what to expect and what treatment paths are available.
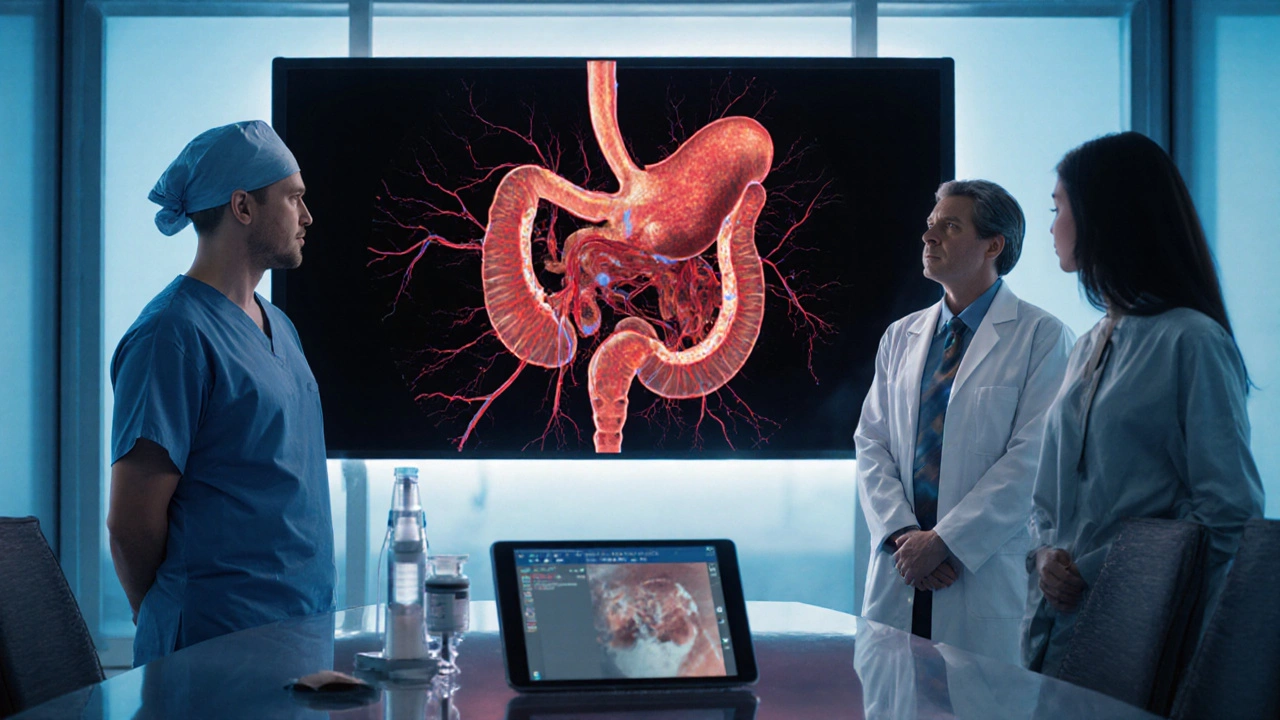
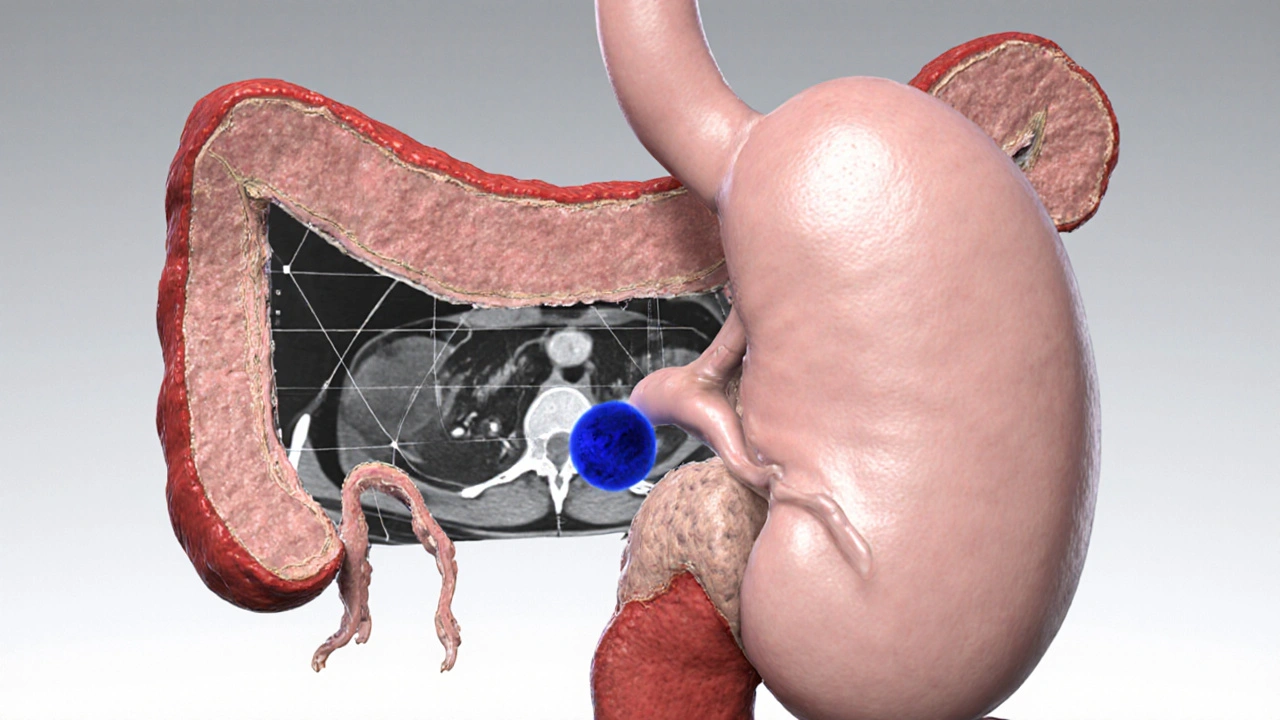
How Doctors Determine the Stage
Accurate staging usually requires a mix of imaging and lab tests. A contrast‑enhanced CT scan generates detailed cross‑sectional images that reveal tumor size and spread. If the CT is inconclusive, a MRI offers higher resolution, especially for vascular involvement. Endoscopic ultrasound (EUS) can obtain fine‑needle biopsies to confirm cancer cells and evaluate nearby lymph nodes.
Blood tests for the tumor marker CA 19‑9 often rises with pancreatic cancer, helping track disease burden. While not definitive for staging, a high level may hint at advanced disease.
Stage I: Cancer Confined to the Pancreas
Stage I means the tumor is limited to the pancreas and measures 2cm or less (IA) or up to 4cm (IB) without node involvement. Patients may experience vague abdominal discomfort or no symptoms at all. Because the disease is still localized, surgical removal offers the best chance for a cure.
Typical interventions:
- Whipple procedure also called pancreaticoduodenectomy, removes the head of the pancreas, part of the duodenum, bile duct, and sometimes part of the stomach.
- Adjuvant chemotherapy, often with gemcitabine a nucleoside analog that slows tumor growth.
Five‑year survival for stageI can reach 25‑30% when surgery is successful and followed by chemotherapy.
Stage II: Tumor Grows Beyond the Pancreas but No Distant Spread
Stage II is split into IIA (tumor extends beyond the pancreas but no lymph node involvement) and IIB (lymph nodes positive). Common signs include jaundice, weight loss, and new‑onset diabetes.
Treatment approach:
- Resection-most patients still qualify for the Whipple or a distal pancreatectomy if the tumor sits in the body/tail.
- Adjuvant chemotherapy, frequently gemcitabine plus capecitabine, improves microscopic clearance.
- Consideration of neoadjuvant therapy (chemo‑radiation before surgery) for borderline‑resectable cases.
Overall five‑year survival hovers around 15‑20% after combined surgery and systemic therapy.
Stage III: Local Advancement With Major Vessel Involvement
Stage III indicates the tumor has invaded major arteries (e.g., celiac axis, superior mesenteric artery) or extensive nodal spread, making immediate surgery unsafe. Symptoms intensify: persistent abdominal pain, severe jaundice, and sometimes pancreatitis.
Management strategy:
- Neoadjuvant chemoradiation (FOLFIRINOX or gemcitabine‑nab‑paclitaxel) to shrink the tumor.
- Re‑assessment for possible surgical resection once vascular involvement lessens.
- If still unresectable, focus shifts to systemic therapy and radiation for local control.
Five‑year survival drops to 5‑10% but aggressive multimodal therapy can extend median overall survival to 12‑18 months.
Stage IV: Metastatic Disease
Stage IV means cancer has spread to distant organs, most often the liver, peritoneum, or lungs. Patients frequently report severe weight loss, persistent pain, and markedly elevated CA 19‑9.
Therapeutic goals:
- Palliation-relieve symptoms, maintain quality of life.
- Systemic chemotherapy (FOLFIRINOX or gemcitabine‑nab‑paclitaxel) to slow disease progression.
- Targeted radiotherapy or stereotactic body radiotherapy (SBRT) for painful liver lesions.
- Early referral to palliative‑care teams for pain management, nutritional support, and psychosocial counseling.
Five‑year survival under 3%; median survival averages 6‑11 months with modern regimens.
Quick Reference Table: Staging at a Glance
| Stage | Tumor Size / Extent (T) | Nodes (N) | Metastasis (M) | Typical Symptoms | 5‑Year Survival (approx.) |
|---|---|---|---|---|---|
| I (IA‑IB) | ≤4cm, confined to pancreas | None | None | Often silent or mild abdominal discomfort | 25‑30% |
| II (IIA‑IIB) | Beyond pancreas, ≤4cm | Negative (IIA) or positive (IIB) | None | Jaundice, weight loss, new diabetes | 15‑20% |
| III | Involves major vessels | Extensive nodal disease | None | Severe pain, refractory jaundice | 5‑10% |
| IV | Any size | Any | Present (liver, lung, peritoneum) | Cachexia, intense pain, high CA19‑9 | <3% |
Living With a Pancreatic Cancer Diagnosis
Beyond the clinical facts, patients need practical advice. Nutrition is critical; a high‑protein, low‑fat diet can help counteract cachexia. Enzyme supplements compensate for reduced pancreatic function. Mental health support-counseling, support groups, or mindfulness apps-reduces anxiety and depression, which are common after a scary diagnosis.
Regular follow‑up imaging (CT every 3‑4 months) tracks response to therapy. Keep a log of symptoms, medication side effects, and CA19‑9 trends to discuss with your oncologist.
Frequently Asked Questions
Can stageI pancreatic cancer be cured?
When the tumor is truly confined (stageI) and a complete surgical resection is achieved, many patients become long‑term survivors. Adjuvant chemotherapy improves the odds, but "cure" depends on clear margins and no microscopic spread.
What does a rising CA 19‑9 level mean?
A rising CA19‑9 often signals tumor growth or recurrence, especially after treatment. However, infections, cholangitis, or biliary obstruction can also elevate the marker, so doctors interpret it alongside imaging.
Is chemotherapy always required?
For stagesI‑II that are surgically removed, adjuvant chemotherapy is standard to kill hidden cells. In stageIII‑IV, systemic therapy is the mainstay because surgery alone cannot control the disease.
Can a patient with stageIII become a surgical candidate?
Yes. If neoadjuvant chemoradiation shrinks the tumor enough to clear major vessels, surgeons may attempt a resection, which can extend survival significantly.
What palliative options exist for stageIV?
Pain management (opioids, celiac plexus block), biliary stenting to relieve jaundice, targeted radiation for bone or liver lesions, and hospice care for end‑of‑life comfort are key components of stageIV care.
Hang in there, every tiny step counts.
The delineation of pancreatic cancer stages provides a crucial framework for clinicians. Understanding the TNM classification allows for precise treatment planning. Early-stage disease, particularly Stage I, often benefits from surgical resection with curative intent. As the tumor progresses to Stage II and III, multimodal therapy becomes essential. Ultimately, Stage IV requires a focus on palliation and quality of life.
Honestly this guide is just another run‑of‑the‑mill overview it adds nothing new and feels like filler
From a TNM perspective, the T1‑T4 descriptors correlate directly with resectability potential. When lymph node involvement (N1‑N2) is detected, adjuvant chemotherapy gains prominence. Vascular encasement, especially of the SMA, often dictates whether neoadjuvant protocols are warranted. Imaging modalities such as contrast‑enhanced CT and MRI furnish the granularity needed for surgical mapping. Molecular profiling, including KRAS and SMAD4 status, may further refine therapeutic choices.
While the article is undeniably informative, one must observe that the terminology employed is occasionally inconsistent; for instance, "locally advanced" versus "locally advanced disease" could be unified, thereby enhancing clarity; likewise, the survival statistics would benefit from citation of peer‑reviewed sources, ensuring verifiability.
Wow, this breakdown really lights a fire under the subject! The colorful stage colors make the data pop, and the survival numbers are both sobering and motivating. It’s brilliant how the guide pairs each stage with a clear treatment pathway. Readers will definitely feel empowered to ask their doctors the right questions. Keep the awesome content coming!
Did you know the whole staging thing might just be a cover for pharma profits they hide the real cure behind layers of bureaucracy
Understanding the nuances of pancreatic cancer staging is absolutely vital for patients and clinicians alike. Each stage not only reflects the anatomical spread but also dictates the therapeutic arsenal available. Stage I, where the tumor is confined and ≤ 2 cm, offers the most hopeful prognosis; surgical resection, such as the Whipple procedure, can be curative. Transitioning to Stage II, the tumor grows beyond 2 cm yet remains localized, often necessitating a combination of surgery, chemotherapy, and sometimes radiation to achieve optimal outcomes. When cancer breaches regional lymph nodes in Stage III, multidisciplinary care becomes paramount; neoadjuvant chemotherapy may precede an attempt at surgical removal, albeit with lower success rates. Stage IV, characterized by distant metastases to organs like the liver or lungs, shifts the treatment focus toward palliation, extending survival while preserving quality of life through systemic therapies and supportive care. Imaging modalities-high‑resolution CT, MRI, and endoscopic ultrasound-play a critical role in accurate staging, enabling clinicians to tailor interventions precisely. Tumor markers, particularly CA 19‑9, provide additional biochemical insight, although they are not definitive on their own. Moreover, emerging genetic profiling can uncover actionable mutations, opening doors to targeted therapies that were unimaginable a decade ago. It’s essential for patients to stay informed, ask questions, and consider second opinions, especially when navigating complex treatment decisions. Support networks, both online and offline, offer emotional reinforcement, helping patients cope with the psychological burden of a diagnosis. Nutrition and lifestyle adjustments, while not curative, can enhance tolerance to aggressive treatments and improve overall well‑being.
Finally, hope remains a steadfast companion; research advances continue to push the boundaries of what’s possible in early detection and innovative therapeutics. Stay proactive, stay hopeful, and remember that every ounce of knowledge empowers you in this challenging journey.
Great points, especially about the genetics-those details can really change the game.
Nice summary! 👍👍
The integration of multimodal therapy in Stage III reflects a sophisticated understanding of oncologic principles, yet the real‑world implementation often suffers from resource constraints and inter‑disciplinary coordination challenges.
Yo this is lit, love the vibe! Real talk, stage stuff is heavy but gotta keep pushin'.
Totally get where you’re coming from, and it's worth noting that the emotional roller‑coaster patients experience often parallels the clinical complexity. While the medical community focuses on metrics and protocols, the human side-fear, hope, family dynamics-can’t be sidelined. It reminds me of a conversation I had with a survivor who said the most valuable thing was a simple, honest chat with their doctor about what each stage truly meant for daily life. Also, the role of nutrition, mental health support, and community resources is frequently under‑emphasized in standard guides. So, when we talk about staging, let’s also advocate for holistic care models that integrate palliative services early on, not just at the nadir. In practice, this could look like regular psychosocial assessments, insurance navigation assistance, and peer‑support group referrals. Ultimately, bridging the gap between clinical data and lived experience may improve adherence and outcomes. Stay kind, stay informed, and keep pushing for that comprehensive approach.
Sounds like the whole system's a big cover‑up, you never know what’s really being hidden.
Oh sure, because the medical community is *totally* in on a grand conspiracy… 🙄