Millions of people take medications every day without issue. But for some, even a common pill can trigger a dangerous reaction. A drug allergy isn’t just a side effect-it’s your immune system overreacting to a medicine, treating it like a threat. And that reaction can be mild… or life-threatening. The problem? Most people don’t know the difference between a harmless side effect and a real allergy. And mislabeling yourself as allergic can cost you more than just a headache-it can lead to worse treatments, longer hospital stays, and even avoidable deaths.
What Does a Drug Allergy Actually Look Like?
- Skin rash - Often the first and most common sign. It can be flat, red spots or raised, itchy welts (hives). These usually show up days after starting the drug, but sometimes within hours.
- Itching - Not just a little itch. Think intense, widespread, and unrelenting. It can happen with or without a visible rash.
- Swelling - Lips, tongue, throat, or eyelids. This isn’t just puffiness. If your throat is swelling, you’re in danger.
- Breathing trouble - Wheezing, coughing, or feeling like you can’t get enough air. This is a red flag.
- Stomach issues - Vomiting, diarrhea, or cramping. Alone, these might seem like the flu. But paired with a rash or swelling? That’s a warning.
When Is It an Emergency? The Signs You Can’t Ignore
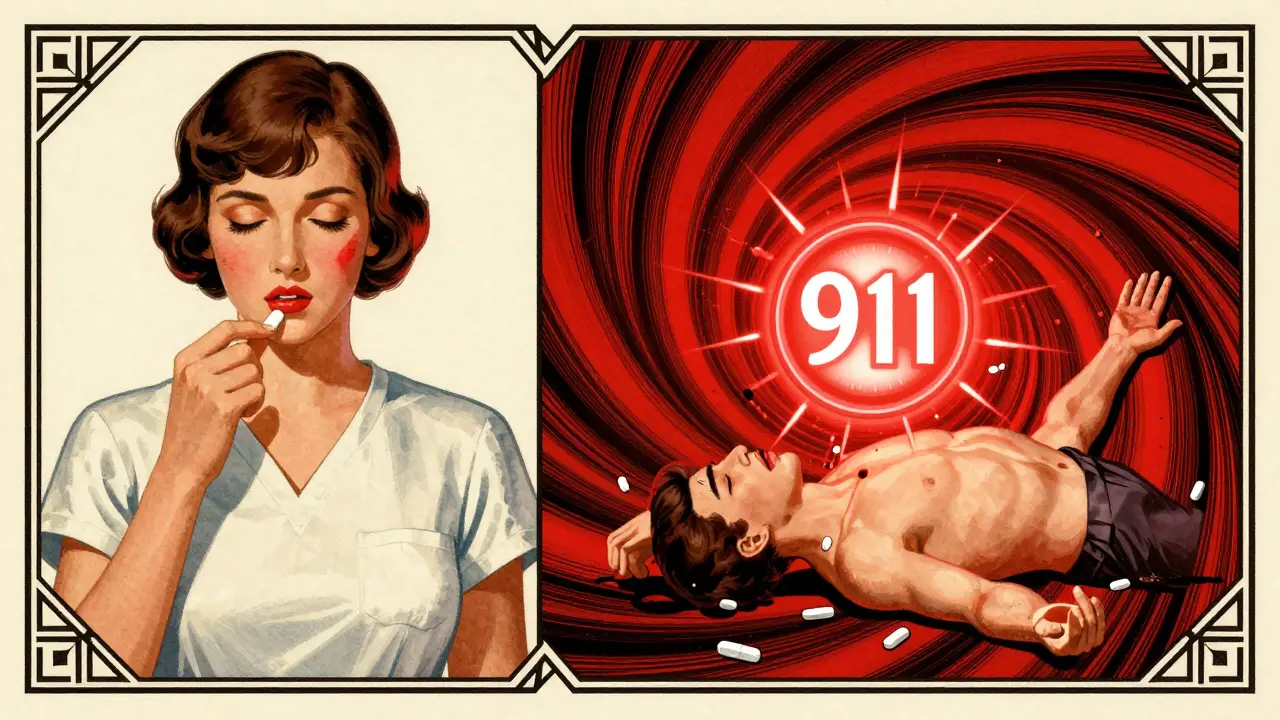
Anaphylaxis is the scariest drug reaction. It’s not just one symptom-it’s two or more body systems crashing at once. Think: skin rash + trouble breathing + swelling + vomiting. This isn’t something you wait out. This is a 911 situation. Here’s what anaphylaxis looks like in real time:- Your skin breaks out in hives or turns pale or blue
- Your throat feels like it’s closing. You can’t swallow or speak clearly
- Your chest tightens. Breathing becomes shallow and fast
- You feel dizzy, lightheaded, or like you’re about to pass out
- Your stomach cramps violently, and you vomit or have diarrhea
Not All Reactions Are Immediate-Watch for Delayed Signs
Some drug allergies don’t strike right away. They sneak up. You take the medicine. You feel fine. Days or even weeks later, something feels off.- Drug rash with eosinophilia and systemic symptoms (DRESS) - Starts as a red, peeling rash, then brings fever, swollen lymph nodes, liver inflammation, and a spike in white blood cells. It can mimic the flu at first, but it’s serious. Left untreated, it can damage your organs.
- Serum sickness-like reaction - Fever, joint pain, swollen glands, and a rash that looks like hives. Usually shows up 1 to 3 weeks after starting the drug.
- Stevens-Johnson Syndrome (SJS) or Toxic Epidermal Necrolysis (TEN) - Rare, but deadly. Begins with flu-like symptoms, then blisters form on your skin and mucous membranes (mouth, eyes, genitals). Large sheets of skin start peeling off. This is a burn-level emergency. Hospitalization is required.
Penicillin Allergy: The Most Common Mislabel
About 10% of Americans say they’re allergic to penicillin. But studies show more than 90% of them aren’t. Why? Because they had a rash as a kid, or felt nauseous after taking it, or someone in their family was allergic. None of those are true allergies. A real penicillin allergy causes hives, swelling, or anaphylaxis. Nausea? That’s a side effect. A mild rash? Could be viral. But once you’re labeled “penicillin-allergic,” doctors avoid it-even when it’s the best, safest, cheapest option. That means you get stronger, costlier antibiotics that increase your risk of deadly infections like C. diff. If you think you’re allergic to penicillin, talk to an allergist. They can test you with a simple skin prick and, if needed, a controlled oral challenge. Most people pass. And if you do? You can go back to using the right drug, not just a backup.What to Do If You Suspect a Drug Allergy
If it’s an emergency (anaphylaxis):- Call 911 immediately
- If you have an epinephrine auto-injector (EpiPen), use it now
- Stay lying down with legs elevated until help arrives
- Stop taking the drug
- Take a photo of the rash or reaction-this helps your doctor diagnose it
- Write down: When did you take the drug? What did you feel? How long did it last?
- Schedule an appointment with your doctor or an allergist
How Doctors Diagnose Drug Allergies (And Why It’s Hard)
There’s no blood test for most drug allergies. Unlike pollen or peanuts, there’s no simple lab test that says “yes, you’re allergic to amoxicillin.” For penicillin, skin testing works. A tiny drop of the drug is placed on your skin, then lightly pricked. If a raised bump appears, you’re likely allergic. If not, you might get a small oral dose under supervision to confirm. For other drugs, doctors rely on your story. Your history matters more than any test. They’ll ask:- Exactly what happened?
- When did it start after taking the drug?
- Did you take any other meds around the same time?
- Have you had this reaction before?

What Happens After a Diagnosis?
If you’re confirmed to have a drug allergy, you’ll get a medical alert bracelet or card. Your doctor will update your records. You’ll learn to avoid that drug-and sometimes, related ones. For example: If you’re allergic to penicillin, you might also react to amoxicillin or ampicillin. But you can usually take cephalosporins safely, unless you had a severe reaction. You’ll also learn what to do if you’re accidentally exposed. Always carry an epinephrine auto-injector if you’ve had anaphylaxis before. Tell every doctor, dentist, and pharmacist about your allergy-every time. And if you’re not sure? Get tested. Don’t live with a label that might be wrong.Why This Matters More Than You Think
Mislabeling a drug allergy isn’t just a personal inconvenience. It’s a public health issue. In the U.S., adverse drug reactions send over 1.3 million people to the emergency room every year. Many of those are avoidable. People labeled allergic to penicillin get broader-spectrum antibiotics. Those drugs are more expensive. They’re harder on your gut. And they increase your risk of antibiotic-resistant infections. That’s not just your problem-it’s everyone’s. Getting the right diagnosis saves lives. It saves money. It saves you from unnecessary risk. If you’ve ever had a reaction to a drug-even a mild one-don’t brush it off. Don’t assume it’s nothing. Don’t let someone else’s guess become your permanent medical label. Talk to a doctor. Get evaluated. Know the truth.Can you outgrow a drug allergy?
Yes, some people can. Penicillin allergies, in particular, often fade over time. Studies show that up to 80% of people who had a penicillin allergy as a child lose the sensitivity after 10 years. But you shouldn’t assume it’s gone. Always get tested by an allergist before taking the drug again. Never self-test.
Can you have a drug allergy without a rash?
Absolutely. While skin reactions are the most common, some drug allergies show up as breathing trouble, low blood pressure, or severe vomiting and diarrhea-without any rash at all. Anaphylaxis often hits the lungs and heart before the skin shows signs. Never wait for a rash to appear before seeking help.
Are over-the-counter drugs like ibuprofen or acetaminophen safe if I have a drug allergy?
Generally, yes-but not always. If your allergy is to a specific class of drugs (like penicillin), OTC pain relievers are usually fine. But some people react to NSAIDs like ibuprofen or aspirin, especially if they have asthma. If you’ve had a reaction to any medication before, talk to your doctor before taking new OTC drugs, even if they seem harmless.
Can a drug allergy happen the first time you take a medicine?
Yes. While some allergies develop after repeated exposure, your immune system can react the very first time you take a drug. This is especially true with antibiotics, seizure medications, and certain painkillers. You don’t need to have taken it before to be allergic.
If I had a reaction to one antibiotic, am I allergic to all of them?
No. Antibiotics are grouped by chemical structure. A reaction to penicillin doesn’t mean you’re allergic to all antibiotics. You might be fine with azithromycin, doxycycline, or ciprofloxacin. Only a specialist can tell you which ones are safe. Never assume cross-reactivity without testing.
Next Steps: What to Do Today
If you’ve ever had a strange reaction to a medication:- Write down the drug name, date, and symptoms
- Take a photo of any rash or swelling
- Call your doctor and ask: “Could this have been a drug allergy?”
- If it was serious, ask for a referral to an allergist
- Don’t wait for it to happen again
- Ask your doctor about penicillin skin testing
- Find an allergist who specializes in drug allergies
- Get the facts before you refuse a life-saving drug

Bro, I had a rash after taking amoxicillin in 2018 and got labeled allergic forever. Turned out it was just a virus. Last year I finally got tested-turned out I’m fine. Now I’m saving $400 per prescription and not getting those nasty C. diff infections. If you think you’re allergic, get tested. It’s not scary, it’s just smart.
Let me tell you something they don’t want you to know. Big Pharma doesn’t want you to know you can outgrow allergies because then you’d stop buying their expensive antibiotics. They profit off fear. The FDA? They’re in bed with the labs. Skin tests? They cost $200, but if you’re labeled allergic, you’re stuck with $1,200 IV drugs for the rest of your life. They’ve been doing this since the 90s. I’ve got 17 pages of FDA documents proving they suppress data on cross-reactivity. You think your doctor’s helping you? Nah. They’re just reading the script. Get your own bloodwork. Demand a challenge test. Or keep paying the price.
It’s funny how we treat medicine like magic pills, but forget our bodies are ancient systems that adapt. We panic at a rash like it’s a cosmic sign, but ignore the fact that our immune systems were designed to learn, not just scream. Maybe the real allergy isn’t to the drug-it’s to uncertainty. We’d rather carry a label than sit with the discomfort of not knowing. I wonder how many lives we’ve lost not to the drug, but to the fear of questioning it.
Y’all are acting like this is news. In Nigeria, we don’t wait for doctors to tell us. If you break out after a pill, you stop it. Period. No testing needed. You don’t play with your life. And if your doctor says ‘it’s probably not an allergy’? Tell him to check his license. I’ve seen people die from ‘mild rashes’ because someone thought they were being ‘reasonable.’ You don’t need a PhD to know when your body’s screaming. Listen to it.
I had a mild reaction to ibuprofen years ago-just a little itching. I stopped taking it and never thought about it again. But reading this made me realize I never told my dentist. I just said ‘I’m allergic to painkillers.’ That’s lazy. I’m going to call my doctor next week and ask about testing. It’s not about being brave. It’s about being accurate. I owe it to myself to get the facts.
Oh please. You’re all acting like this is some revolutionary insight. I’ve been saying this for years: the medical industrial complex is a scam. You think they care if you get the right antibiotic? Nah. They care if you keep buying their $100 pills. And don’t even get me started on EpiPens-$600 for a plastic injector that’s basically a glorified syringe. Someone’s making bank off your fear. Wake up. This isn’t medicine. It’s marketing.
It is imperative to underscore the gravity of mislabeling drug allergies, as such errors may lead to suboptimal therapeutic outcomes and increased morbidity. The data presented herein aligns with peer-reviewed literature from the Journal of Allergy and Clinical Immunology, which affirms that up to 95% of self-reported penicillin allergies are not confirmed upon formal evaluation. It is therefore strongly recommended that all patients with a history of suspected drug hypersensitivity be referred to a board-certified allergist for comprehensive assessment. This is not merely a personal health consideration-it is a matter of clinical responsibility.
Okay, but what if the real danger isn’t the drug-it’s the system? What if the whole concept of ‘drug allergies’ is a distraction? Think about it. Why do we assume our bodies are broken when they react? Maybe the drugs are the problem. Maybe the chemicals are poisoning us slowly, and our immune systems are the only thing trying to scream ‘STOP!’ They call it an allergy… but what if it’s a warning? What if we’re not allergic to penicillin… we’re allergic to corporate greed disguised as medicine? And they’re gonna test you with a needle and say ‘you’re fine’… while they keep selling you the poison. They don’t want you to question the source. They want you to question your body.
My cousin got mislabeled penicillin-allergic after a stomach bug. Now she’s on clindamycin every time she gets an infection. Got C. diff three times. Last year she finally got tested-turned out she was fine. Now she’s on penicillin again and feels better than ever. Don’t be a statistic. If you think you’re allergic, get tested. It’s a 30-minute appointment. Your future self will thank you.