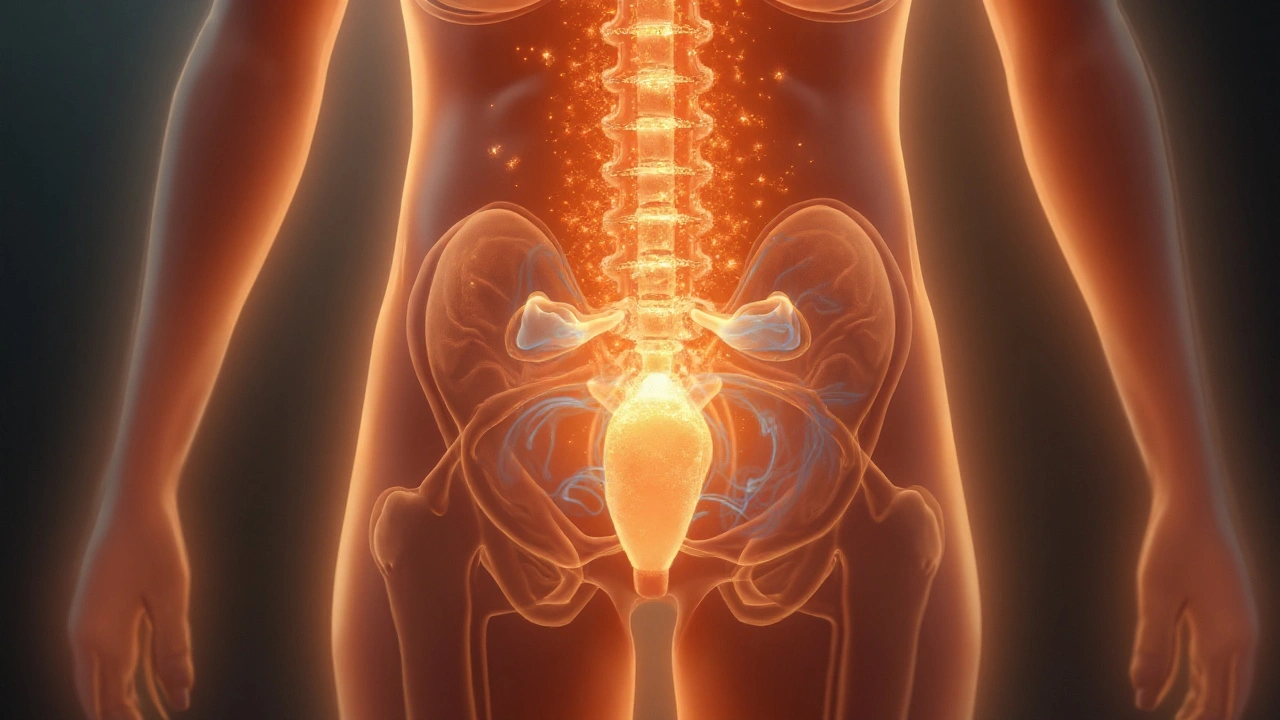
Bladder and urinary tract muscle spasms are involuntary contractions of the detrusor muscle and urethral sphincter that disrupt normal urine flow. In people living with Multiple Sclerosis, these spasms are a hallmark of neurogenic bladder dysfunction, often leading to urgency, incontinence, or retention. Understanding the link helps clinicians and patients choose the right interventions and improve quality of life.
What exactly are bladder muscle spasms?
When the bladder fills, the detrusor muscle should relax, storing urine safely. A spasm occurs when the detrusor contracts prematurely, sending a false signal that the bladder is full. The result is a sudden urge to void, sometimes with only a few drops released. In MS, the brain‑spinal cord communication that tells the detrusor when to contract is scrambled, so the muscle fires off‑schedule.
How Multiple Sclerosis triggers these spasms
Multiple Sclerosis is an autoimmune disease that attacks the myelin sheath protecting nerve fibers in the central nervous system. Demyelination slows or blocks signals traveling between the brain, spinal cord, and peripheral nerves that control the urinary tract. The two most common urodynamic patterns in MS are:
- Detrusor overactivity: involuntary detrusor contractions during the filling phase.
- Detrusor‑sphincter dyssynergia: the bladder pushes while the urethral sphincter stays closed, causing high‑pressure retention.
Both patterns stem from disrupted autonomic pathways. Studies from the National MS Society show that up to 80% of people with MS experience some form of urinary dysfunction within ten years of diagnosis.
Typical symptoms and daily impact
Patients describe the spasms as a “burst” sensation that can’t be ignored. Common complaints include:
- Urgency - a compelling need to pee every few hours.
- Urge incontinence - leaking before reaching the bathroom.
- Frequency - visiting the toilet 8‑12 times a day.
- Nocturia - waking up multiple times at night.
- Retention - feeling the bladder is still full after voiding.
These issues interfere with work, social life, and even sleep, increasing the risk of skin breakdown and urinary tract infections.
How doctors diagnose muscle spasms in MS
Accurate diagnosis hinges on two tools:
- Urodynamic study: measures bladder pressure, flow rates, and sphincter activity. It can differentiate detrusor overactivity from dyssynergia.
- Magnetic Resonance Imaging (MRI): maps lesions in the spinal cord that correlate with urinary symptoms.
Questionnaires such as the International Prostate Symptom Score (IPSS) help quantify subjective bother, while a bladder diary tracks real‑world patterns.
Management options - from lifestyle tweaks to advanced therapies
Choosing a treatment depends on symptom severity, bladder capacity, and personal goals. Below is a tiered approach:
- Behavioral strategies: timed voiding, bladder training, and fluid management.
- Pharmacologic agents:
- Anticholinergic medication (e.g., oxybutynin) relaxes the detrusor but may cause dry mouth.
- Beta‑3 agonists (mirabegron) boost bladder storage without the anticholinergic side‑effects.
- Injectable therapy: Botulinum toxin (Botox) injected into the detrusor reduces overactivity for 6‑9 months; ideal for refractory cases.
- Catheterisation: Intermittent catheterisation empties the bladder safely when retention is dominant.
- Surgical options: sphincterotomy or bladder augmentation, reserved for severe, unresponsive cases.
All treatments aim to protect the upper urinary tract, prevent infections, and restore confidence.

Comparison of the two most common spasm patterns
| Attribute | Detrusor Overactivity | Detrusor‑Sphincter Dyssynergia |
|---|---|---|
| Prevalence in MS | ≈ 65% | ≈ 30% |
| Typical symptom | Urgency & urge incontinence | Incomplete emptying, high‑pressure retention |
| Urodynamic finding | Spontaneous detrusor contractions during filling | Detrusor contraction with simultaneous sphincter contraction |
| First‑line treatment | Anticholinergics or beta‑3 agonists | Intermittent catheterisation + possible botulinum toxin |
| Risk if untreated | UTIs, bladder wall thickening | Upper‑tract damage, renal failure |
Deciding which therapy fits your life
Think of treatment choice like a decision tree. Ask yourself:
- Is urgency the main issue? Try anticholinergics first.
- Do you often feel the bladder is still full? Intermittent catheterisation may be necessary.
- Are side‑effects intolerable? Consider beta‑3 agonists or Botox.
- Is your bladder capacity < 150mL? Surgical referral might be warranted.
Collaborate with a urologist or neuro‑urology specialist who can interpret urodynamic data and adjust therapy as the disease evolves.
Living with bladder spasms - practical tips
- Keep a small portable urinal or pads in your bag - it reduces anxiety.
- Stay hydrated, but avoid excess caffeine and alcohol, which can trigger overactivity.
- Schedule bathroom breaks every 2-3hours rather than waiting for the urge.
- Pelvic floor physical therapy can improve sphincter coordination for some patients.
- Track infections promptly; early antibiotics prevent kidney damage.
People often underestimate the emotional toll. Joining an MS support group gives you a safe space to share tricks and stay motivated.
Related concepts you might explore next
If you found this guide useful, consider reading about these adjacent topics:
- Neurogenic bowel dysfunction in Multiple Sclerosis
- Impact of disease‑modifying therapies on urinary symptoms
- Advances in wearable bladder monitoring technology
- Psychological coping strategies for chronic illness
Each builds on the idea that managing MS is a multi‑system effort, and bladder health is just one piece of the puzzle.
Frequently Asked Questions
Why do bladder spasms happen early in MS?
Lesions often appear first in the spinal cord segments that control the sacral nerves. When those pathways are damaged, the brain can’t reliably tell the bladder when to store or release urine, leading to early overactivity.
Can anticholinergic meds worsen MS symptoms?
In some people, anticholinergics cause cognitive fog or constipation, which can feel like MS flare‑ups. If you notice these side‑effects, talk to your doctor about dose adjustment or switching to a beta‑3 agonist.
Is Botox safe for long‑term use?
Clinical trials spanning ten years show that repeated Botox injections keep detrusor overactivity controlled without increasing the risk of urinary retention, as long as injections are spaced 6‑9 months apart and monitored by urodynamics.
When should I consider intermittent catheterisation?
If post‑void residual volumes regularly exceed 150mL or you experience frequent urinary tract infections, intermittent catheterisation is recommended to protect your kidneys and reduce infection risk.
Do lifestyle changes really help?
Yes. Timed voiding, fluid timing, and pelvic floor exercises have been shown in real‑world studies to cut urgency episodes by up to 40% and improve quality‑of‑life scores.
They don’t tell you that the pharma companies are pushing these “new therapies” to keep us hooked on endless prescriptions, all while hiding the real cause of bladder spasms in the shadowy labs. The whole system is a racket, and patients are left scrambling for relief.
OMG, the drama is real!! But yu really think the gov is behind urny smarts? It’s just a normal med clincal trial, not some secret plot.
I've seen many folks coping with these spasms and honestly, small lifestyle tweaks can make a big difference 😊. Timing your bathroom trips and staying hydrated (but not over‑caffeinated) helped my friend cut urgency episodes by half.
Exactly! Leveraging voiding schedules aligned with urodynamic findings-specifically targeting detrusor overactivity-optimizes bladder capacity. Engaging in pelvic‑floor muscle training also enhances sphincter coordination, which can attenuate dyssynergia events.
The bladder, that humble reservoir, becomes a metaphor for the constraints we place upon ourselves in the face of chronic illness; When neurons misfire, the detrusor muscle erupts in rebellion, an involuntary reminder that the body does not always heed the mind’s commands; This dissonance mirrors the philosophical tension between free will and determinism, a theme explored by thinkers from Aristotle to Sartre; In multiple sclerosis, demyelinated pathways scramble signals, turning longing for control into urgent, often embarrassing, sensations; One might argue that the urgency is a call to mindfulness, urging sufferers to be present in the now, even as the body protests; Yet, the clinical reality demands pragmatic interventions-anticholinergics, beta‑3 agonists, or even Botox-to restore functional equilibrium; Each therapeutic option carries its own ethical considerations, balancing efficacy against side‑effects such as dry mouth or cognitive fog; The physician, therefore, becomes a steward of choice, guiding patients through a labyrinth of data, personal values, and societal expectations; Meanwhile, the patient navigates a landscape of stigma, where nocturia and incontinence can erode confidence and social participation; Social support networks, both offline and online, act as bulwarks against isolation, offering practical tips and emotional solace; Moreover, advances in wearable bladder monitoring promise to quantify patterns, transforming subjective diaries into objective metrics; Such technology, however, raises questions about privacy, data ownership, and the commodification of intimate bodily functions; Ultimately, the journey through bladder spasm management in MS is a microcosm of the broader human quest for agency amid uncertainty; It teaches us that resilience is not the absence of symptoms, but the capacity to adapt, seek help, and reframe adversity; In this light, every scheduled void, every catheter change, and every medication adjustment becomes a step toward reclaimed dignity.
Honestly, if you keep ignoring the basics like fluid timing and pelvic exercises, you're just sabotaging yourself. It's not just a medical thing, it's about taking responsibility for your own health.
We all learn at our own pace, and sharing tips across communities can help everyone feel supported.
From a urology perspective, intermittent catheterisation reduces post‑void residual volume to <150 mL, which markedly lowers the risk of upper‑tract deterioration. Pair that with periodic urodynamic assessments, and you have a data‑driven roadmap for symptom control 😊.
The comprehensive approach outlined in the article aligns well with current best‑practice guidelines, integrating behavioral, pharmacologic, and procedural strategies to address both detrusor overactivity and dyssynergia. Its emphasis on patient‑centered decision making reflects an encouraging shift toward individualized care.
While the article praises a balanced regimen, one must consider that many of these “guidelines” are heavily influenced by pharmaceutical lobbying; the so‑called “best‑practice” often masks profit‑driven agendas, and patients should remain skeptical of any blanket recommendations.
It is utterly reprehensible that anyone would settle for sub‑optimal bladder management when evidence‑based protocols exist; mediocrity in care is a moral failing that we must condemn with unequivocal resolve.
Although the piece is thorough, it neglects to address the socioeconomic barriers that prevent many patients from accessing advanced therapies, a glaring omission in an otherwise comprehensive review.
The article correctly lists treatment options, but it fails to prioritize them based on cost‑effectiveness; without this, clinicians may overprescribe expensive drugs that offer minimal benefit.