When you’re on a blood thinner, the goal isn’t just to prevent clots-it’s to do it without bleeding out. For millions of people with atrial fibrillation, deep vein thrombosis, or mechanical heart valves, choosing between warfarin and direct oral anticoagulants (DOACs) isn’t just a medical decision. It’s a life-altering one.
Warfarin: The Old Standard with a Heavy Burden
Warfarin has been around since 1954. It works by blocking vitamin K, which your body needs to make clotting factors. Sounds simple, right? But here’s the catch: every little thing you eat, drink, or take as a pill can throw it off. A handful of spinach, an antibiotic, even a change in your sleep schedule can send your INR-your blood’s clotting time-skyrocketing or crashing. Doctors used to rely on weekly blood tests to keep your INR between 2.0 and 3.0. Too low, and you’re at risk for a stroke. Too high, and you could bleed internally without warning. Studies show that even under ideal conditions, patients spend less than 70% of their time in the safe range. In real life? It’s often worse. Many people miss appointments, forget to get tested, or can’t afford the travel or time off work. And the interactions? Over 300 drugs and countless foods interfere with warfarin. Grapefruit juice? Bad. St. John’s wort? Worse. Even switching from one brand of generic warfarin to another can cause instability. That’s why the FDA requires a Risk Evaluation and Mitigation Strategy (REMS) program just to prescribe it.DOACs: The New Kids on the Block
Enter DOACs-apixaban, rivaroxaban, dabigatran, and edoxaban. These drugs don’t mess with vitamin K. Instead, they target specific clotting proteins directly: factor Xa or thrombin. That means no more weekly INR checks. No more dietary restrictions. No more guessing. In 2023, DOACs made up nearly 78% of all anticoagulant prescriptions in the U.S. Apixaban (Eliquis) alone accounted for 38.5% of the market. Why? Because the data speaks for itself. A 2023 study in JAMA Network Open found that for people with atrial fibrillation, DOACs lowered the risk of stroke by 30% and major bleeding by 28% compared to warfarin. Intracranial bleeding-the kind that can kill you overnight-dropped by more than half. And in patients with kidney disease down to an eGFR of 25 mL/min, DOACs still outperformed warfarin in safety. The biggest win? Adherence. A 2023 study in the American Journal of Managed Care showed DOAC users were 32% more likely to take their medication consistently. For younger adults, that gap jumped to 41%. Why? Because life doesn’t stop for blood tests.But DOACs Aren’t Perfect
They’re safer-but not risk-free. And they’re expensive. A 30-day supply of apixaban costs around $587. Warfarin? $4.27. That’s not a typo. For people without good insurance, the price difference is a dealbreaker. Some DOACs also have limits. Dabigatran is mostly cleared by the kidneys, so it’s risky if your eGFR drops below 30. Rivaroxaban and edoxaban aren’t recommended if your kidney function is below 15 mL/min. Apixaban handles kidney issues better than the others, making it the go-to for patients with mild to moderate renal impairment. And here’s something rarely talked about: reversal agents. If you bleed badly, you need something to stop the drug fast. For dabigatran, there’s idarucizumab (Praxbind). For apixaban and rivaroxaban, there’s andexanet alfa (Andexxa). But these drugs cost thousands per dose. Not every hospital stocks them. And they’re not magic-once you’ve lost a liter of blood, no reversal agent brings it back.
Who Still Needs Warfarin?
Not everyone can switch. If you have a mechanical heart valve, DOACs are dangerous. They don’t work well there-and using them can lead to valve clots, strokes, or death. Warfarin is still the only proven option. Same goes for severe kidney failure-specifically dialysis-dependent patients. While some newer studies suggest DOACs may be safer even here, guidelines still recommend warfarin because the data isn’t solid enough. The KDIGO guidelines from 2023 say: stick with warfarin until more evidence comes in. Patients with severe mitral stenosis or certain types of heart valve disease also need warfarin. Dr. Steven A. Lubitz from Massachusetts General Hospital says it plainly: “For these patients, warfarin is the only proven option.”Real People, Real Choices
On patient forums like Blood-Thinners.com, 78% of 1,245 users said they’d pick DOACs again. Why? “No more spinach anxiety,” said one user. “I can eat a salad without checking my INR.” Another: “I don’t have to take a day off work every month for a blood draw.” But then there’s the cost. One Reddit user wrote: “I’m on warfarin because I can’t afford Eliquis. I do the tests. I count my greens. I’m tired. But I’m alive.” For older adults with stable INRs and good access to clinics, warfarin still works. For younger, busy people-especially those with jobs, kids, or no insurance-DOACs are life-changing.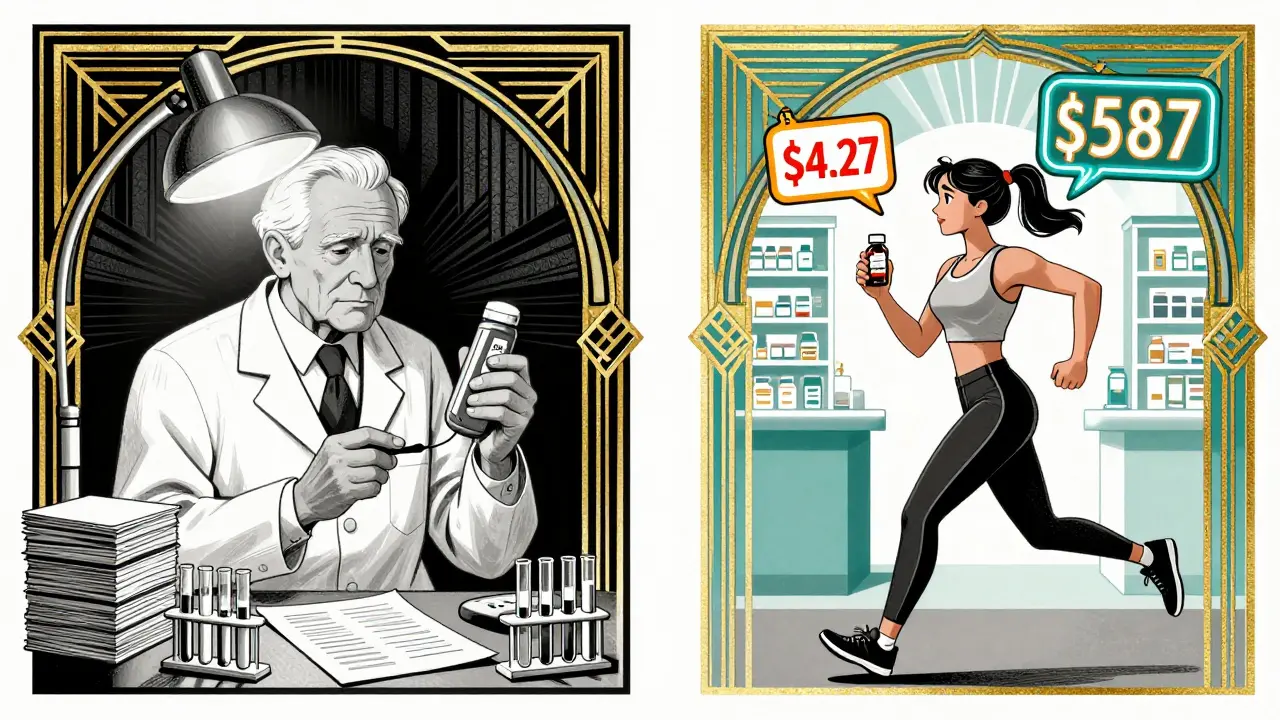
What Should You Do?
If you’re on warfarin and doing well-with regular tests, stable INRs, and no major bleeding-you might not need to switch. But if you’re struggling with diet restrictions, frequent blood draws, or unpredictable results, talk to your doctor about DOACs. If you’re starting anticoagulation now, DOACs are the first-line choice for most people-with a few exceptions:- Choose DOACs if you have non-valvular atrial fibrillation, DVT, or PE and no major kidney issues.
- Stick with warfarin if you have a mechanical heart valve, severe mitral stenosis, or are on dialysis.
- For kidney impairment (eGFR 25-59), apixaban is usually the safest DOAC.
- Avoid DOACs if your eGFR is below 15 mL/min.
What’s Coming Next?
Researchers are testing new combos like Librexia™-a pill that blends warfarin with vitamin K to stabilize dosing. If it works, it could make warfarin easier to use again. The AUGUSTUS-CKD trial, due to finish in late 2024, will finally answer whether DOACs are safe for dialysis patients with atrial fibrillation. Until then, caution rules. Market trends show DOACs will hit 85% of the anticoagulant market by 2028. But warfarin won’t disappear. It’s too cheap, too well-understood, and too essential for specific cases. The bottom line? There’s no one-size-fits-all blood thinner. Safety depends on your kidneys, your heart, your wallet, and your life. The best choice isn’t the newest drug-it’s the one that fits your body and your life.Are DOACs safer than warfarin?
Yes, for most people. DOACs reduce the risk of stroke and major bleeding by 20-30% compared to warfarin. They don’t need frequent blood tests and have fewer food and drug interactions. But they’re not safer for everyone-people with mechanical heart valves or very severe kidney disease still need warfarin.
Can I switch from warfarin to a DOAC?
Many people can, but it’s not automatic. Your doctor will check your kidney function, type of condition (like atrial fibrillation or mechanical valve), and whether you’ve had bleeding before. If you’re stable on warfarin with good INR control, switching might not be necessary. But if you’re struggling with diet, testing, or side effects, DOACs are often a better fit.
Why are DOACs so expensive?
DOACs are brand-name drugs with limited generic competition. Apixaban and rivaroxaban still have patent protections in many countries. Warfarin is old, off-patent, and made by dozens of manufacturers. A 30-day supply of warfarin costs about $4. DOACs cost $500 or more. Some insurance plans cover them, but copays can still be high. Patient assistance programs exist-ask your pharmacist.
Do I need to get blood tests if I’m on a DOAC?
Routine blood tests aren’t needed for DOACs like they are for warfarin. But your doctor will still check your kidney function (eGFR) at least once a year. In emergencies-like major bleeding or before surgery-special blood tests can measure DOAC levels. These aren’t for daily use, just for urgent situations.
What happens if I miss a dose of a DOAC?
DOACs have a short half-life, so missing a dose can leave you unprotected faster than with warfarin. If you miss a morning dose, take it as soon as you remember-if it’s still the same day. If it’s almost time for your next dose, skip the missed one. Never double up. Unlike warfarin, there’s no buffer from lingering drug in your system. Consistency matters more with DOACs.

Man, I remember when my grandma was on warfarin-she had this little notebook where she logged every spinach salad like it was a military operation. I used to joke she was running a food intelligence unit. Then she switched to Eliquis and just… stopped worrying. No more weekly trips to the clinic. No more ‘is this avocado gonna kill me?’ anxiety. Life got lighter. Not just medically-emotionally too.
The pharmacokinetic superiority of DOACs over vitamin K antagonists is statistically and clinically unambiguous. The reduction in intracranial hemorrhage-HR 0.47, 95% CI 0.39–0.56-isn't just a trend, it's a paradigm shift. The fact that we're still debating this in 2025 speaks to systemic healthcare inertia rather than clinical ambiguity. We're clinging to a 1954 algorithm in an era of precision medicine.
It’s not just about blood tests or spinach. It’s about autonomy. Warfarin turns you into a patient. DOACs let you be a person. I used to dread weekends because I knew Monday meant another blood draw. Now? I eat tacos at 2 a.m. and sleep like a baby. I didn’t just gain convenience-I regained my dignity. And yes, it’s expensive. But what’s the cost of losing your life to fear?
Let’s be real-DOACs aren’t magic. They’re expensive, reversible only if your hospital has a $15k vial sitting in the freezer, and if you’re over 75 with borderline renal function? You’re playing Russian roulette with a 30% chance of GI bleeds. And don’t get me started on the fact that 80% of prescribers don’t even know the half-life differences between apixaban and rivaroxaban. We’re replacing one problem with a more expensive, less understood one. The FDA pushed these because they’re profitable, not because they’re universally better.
My uncle died from a GI bleed on rivaroxaban. No reversal agent available. No time. Just… gone. The data says ‘safer.’ Real life says ‘it depends.’
People act like DOACs are the answer to everything. But if you’re poor, you’re still stuck with warfarin. And let’s be honest-most of these ‘studies’ are funded by pharma. Who’s to say the real-world bleeding rates aren’t higher because people skip doses and think ‘it’s fine, no labs needed’? The system rewards convenience over responsibility. And now we’re punishing the poor for not being able to afford the new toy.
As someone from India, I’ve seen both sides. My father was on warfarin for 12 years-weekly INR, strict diet, constant anxiety. Then we found a patient assistance program for apixaban. He cried the first time he ate a mango without checking his INR. DOACs saved his life-not because they’re perfect, but because they gave him peace. Yes, cost is a barrier. But that’s not a flaw in the drug-it’s a flaw in the system. We need better access, not less innovation.
My mom’s on warfarin and she’s 82. Stable INR. No bleeding. She goes to the clinic every week and chats with the nurse like they’re old friends. She doesn’t want to switch. Why? Because she knows her body, she trusts the routine, and the cost of switching isn’t worth it for her. Not everyone needs to be ‘modernized.’ Sometimes stability is the real win.
DOACs are a corporate scam wrapped in a clinical trial. Warfarin is dirt cheap. DOACs cost $600 a month. That’s not medicine-that’s extortion. And the reversal agents? More expensive than a used car. We’re not saving lives-we’re creating a new class of patients who are dependent on pharmaceutical oligarchs. If you’re not outraged by this, you’re not paying attention.
And don’t tell me ‘it’s safer.’ My cousin bled out on apixaban because the ER didn’t have Andexxa. He was 52. He had a kid. The system failed him. And the pharma reps are still out there handing out pens with Eliquis logos.
warfarin is fine if you dont mind being a lab rat. doacs are better but only if you have insurance. if you dont? good luck. also who even checks eGFR yearly? no one. so yeah. we’re all just guessing.
So let me get this straight-we replaced a drug that requires monitoring with a drug that requires… nothing? And we call that progress? What happens when someone forgets a dose for three days? Suddenly they’re a walking clot factory. Warfarin at least gives you a warning sign. DOACs? Silent until you collapse. And we’re praising this as ‘convenient’? It’s just risk displacement.
For those of us who’ve been on the front lines-ER nurses, paramedics, primary care docs-this isn’t theoretical. I’ve seen patients on DOACs bleed out because no one knew how to manage it. I’ve seen warfarin patients stabilize because their INR was tracked religiously. The answer isn’t ‘DOACs good, warfarin bad.’ It’s ‘match the tool to the person.’ And that requires time, education, and resources we’re not investing in. We’re treating this like a product launch, not a medical decision.
The ethical dimension of this choice cannot be overstated. When we prioritize cost-effectiveness over patient autonomy, we are not merely making a pharmacological decision-we are making a moral one. The patient who chooses warfarin not out of preference, but out of economic coercion, is not exercising agency-they are surviving within a system that has commodified health. The fact that we accept this as normal is a failure of our collective conscience. DOACs represent not just a pharmacological advancement, but a societal opportunity: to treat anticoagulation not as a commodity, but as a human right. Until we decouple access from income, we are not healing-we are stratifying.
Let me tell you about Maria. 68, diabetic, on warfarin for AFib. She lives in a rural town with no pharmacy within 40 miles. She walks to the clinic every Monday. Her INR’s been stable for five years. She doesn’t care about the ‘new drugs.’ She cares that her nurse remembers her name, that she gets a free coffee while she waits, that she doesn’t have to choose between her meds and her groceries. Maria’s not a statistic. She’s a person who’s found peace in routine. And if her doctor says ‘stay on warfarin,’ that’s not failure-that’s wisdom. Not everyone needs to chase the shiny thing. Sometimes, the old thing is the right thing-for them.
So before you judge someone for staying on warfarin, ask yourself: would you give up your peace of mind for a 28% lower bleeding risk… if you couldn’t afford it?
I’m the author of this post. Thank you all for the thoughtful, raw, and sometimes angry replies. You’re not just commenting-you’re sharing your lives. That’s what this is really about. I didn’t write this to pick sides. I wrote it because I’ve sat with patients who cried because they couldn’t afford Eliquis. I’ve held hands with families who lost someone because Andexxa wasn’t in stock. This isn’t about which drug is better. It’s about who gets to be safe. And that’s the real question we’re avoiding.