When you're diagnosed with glaucoma, your doctor will likely recommend one of two main types of eye drops: prostaglandins or beta blockers. Both lower eye pressure-the main goal in stopping glaucoma from damaging your vision-but they work in very different ways, and their side effects can change your life in ways you might not expect.
How Prostaglandins Lower Eye Pressure
Prostaglandin analogs like latanoprost, bimatoprost, and travoprost don’t just reduce fluid in the eye-they change how it drains. These medications activate receptors in the eye’s drainage system, opening up new pathways for fluid to escape. This is called uveoscleral outflow. The result? A 24% to 33% drop in eye pressure, often more than any other class of glaucoma drug.
What makes prostaglandins popular isn’t just their power-it’s how easy they are to take. One drop, once a day, usually at night. No reminders. No complicated schedules. That’s why they’re the top first-choice treatment in most clinics today. A 2019 study found that 39% of people stayed on prostaglandins after a year, compared to just 25% on beta blockers.
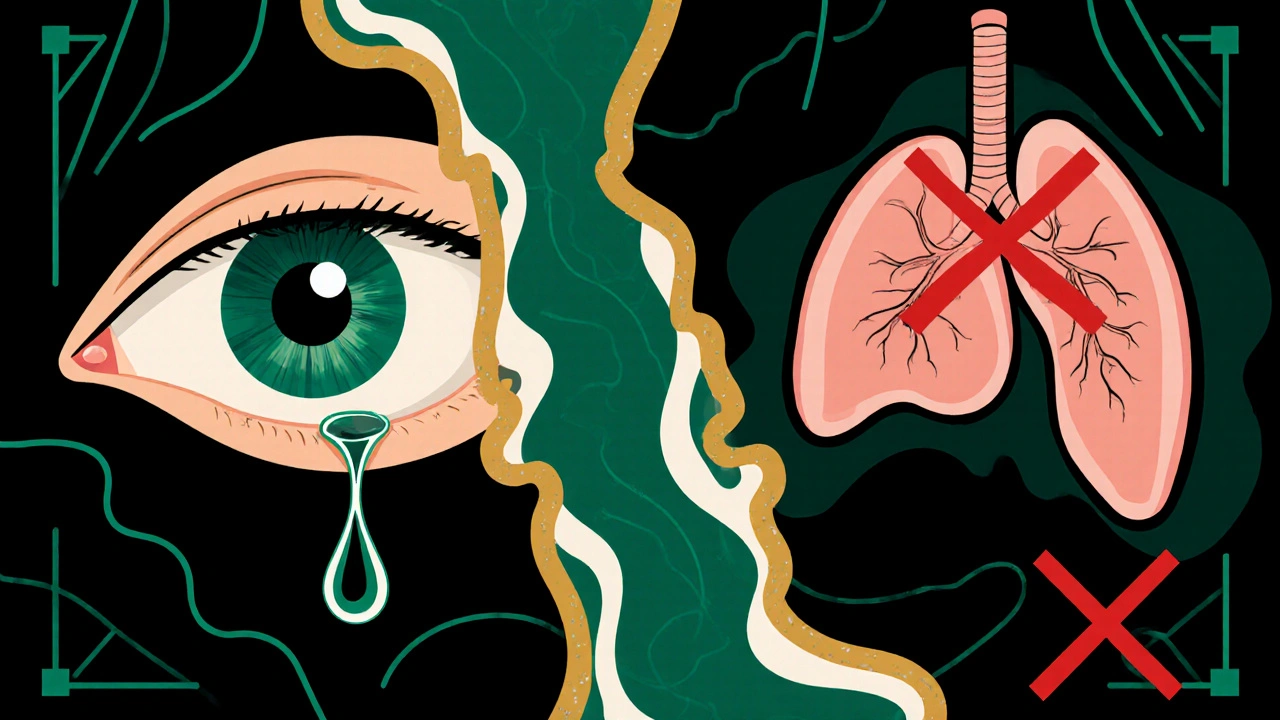
But there’s a catch. These drops cause real, lasting changes to your eyes. About 5% to 10% of long-term users develop darker iris color-especially if they have hazel or green eyes. Eyelashes get longer, thicker, and darker. Some people like this side effect. Others find it unsettling. And while it’s not dangerous, it’s permanent. Once it happens, it doesn’t go away when you stop the drops.
Another common issue: red eyes. Up to half of users notice redness or bloodshot appearance. It’s usually mild and fades during the day, but it can make people self-conscious. Bimatoprost causes more redness and irritation than latanoprost. About 25% to 30% of bimatoprost users report burning or stinging, compared to 15% to 20% with latanoprost. That’s why many doctors start with latanoprost unless there’s a reason to choose otherwise.
How Beta Blockers Work-and Their Hidden Risks
Beta blockers like timolol and betaxolol work differently. Instead of helping fluid drain, they slow down how much fluid your eye makes. They block beta receptors in the ciliary body, the part of the eye that produces aqueous humor. This reduces pressure by about 20% to 25%-slightly less than prostaglandins, but still effective.
Here’s the problem: beta blockers aren’t just local. They get absorbed into your bloodstream. That means they can affect your heart and lungs. If you have asthma, COPD, or a slow heart rate, these drops can be dangerous. They’ve been linked to breathing trouble, fatigue, dizziness, and even heart failure in high-risk patients. The FDA requires a black box warning on timolol for these reasons.
Another downside: you have to use them twice a day. That cuts into adherence. Studies show people forget or skip doses more often with twice-daily meds. One study found that people on beta blockers were 60% more likely to stop taking their drops within a year than those on prostaglandins.
Betaxolol, a selective beta blocker, may be safer for people with mild lung issues because it’s less likely to affect the airways. Some early data suggested it might protect vision better in the first six months than timolol, but that hasn’t held up in longer studies. Still, for patients who can’t use prostaglandins, betaxolol is often the go-to beta blocker.
Which Is Safer? It Depends on You
Safety isn’t just about side effects-it’s about who you are.
If you have asthma, COPD, heart disease, or depression, beta blockers are risky. Even if you’ve never had symptoms, your doctor should check your medical history before prescribing them. If you’re over 65, have diabetes, or take other heart meds, the risk goes up.
If you’re young, healthy, and don’t mind cosmetic changes, prostaglandins are usually the better pick. But if you’re concerned about darkening irises or thickening lashes, or if you work in a job where red eyes are frowned upon (like customer service or photography), you might want to avoid them.
There’s no one-size-fits-all answer. A 2013 seven-year study comparing the two classes found no difference in how well they protected vision. Both kept the visual field stable over time. That means the choice isn’t about which one works better-it’s about which one you can stick with.
Combining Medications: More Isn’t Always Better
Many people end up on more than one drop. If one medication doesn’t lower pressure enough, doctors often add another. Combining a prostaglandin with a beta blocker like timolol can drop pressure an extra 13% to 25%-better than either alone.
But here’s the twist: mixing two prostaglandins (like latanoprost and bimatoprost) can actually raise eye pressure. That’s not a mistake-it’s a known risk. Studies show this combo can make glaucoma worse. Don’t ever do it.
Fixed-dose combinations (like latanoprost/timolol in one bottle) exist to simplify routines. But they’re not always better. A 2005 study found no clear advantage in pressure control over using the drops separately. The real benefit? Fewer bottles, fewer drops, fewer chances to forget.
Preservative-Free Drops: Worth the Extra Cost?
Most glaucoma drops contain benzalkonium chloride (BAK), a preservative that kills bacteria but also damages the eye’s surface over time. Long-term users often develop dry eyes, burning, and irritation.
Preservative-free versions are available for both prostaglandins and beta blockers. A 2021 review of seven studies found they improved tear film quality and reduced dryness. But here’s the catch: they lowered eye pressure by only 0.29 mmHg more than preserved drops-so little that it’s not clinically meaningful.
So why do they cost 20% to 25% more? Because they’re single-use vials. You throw them away after one use. Hospitals and large clinics are starting to use them for long-term patients, especially those with dry eye or contact lens wearers. But for most people, the benefit doesn’t justify the price.

What to Expect When You Start
When you begin either type of drop, your doctor will likely ask you to come back in 4 to 6 weeks. That’s to check your eye pressure and ask about side effects.
Here’s what to watch for:
- Prostaglandins: Red eyes, longer lashes, darker iris color, occasional stinging. These usually start within days or weeks.
- Beta blockers: Fatigue, dizziness, shortness of breath, slow heartbeat, cold hands or feet. These can show up anytime, even months later.
If you notice any of these, don’t stop the drops. Call your doctor. Some side effects can be managed with different timing, different drops, or even switching classes.
Proper technique matters too. Tilt your head back, pull down your lower lid, drop it in, close your eye, and press gently on the inner corner of your eye for a minute. This keeps the medicine from draining into your nose and getting absorbed into your bloodstream-especially important with beta blockers.
Long-Term Outlook: What’s Next?
Glaucoma is a lifelong condition. Medications won’t cure it, but they can stop it from getting worse. For now, prostaglandins are the standard first step for most people. Beta blockers are still used, but mostly when prostaglandins aren’t right-because of cost, side effects, or medical history.
Research is moving toward new delivery systems: slow-release implants, contact lenses that release medicine, and even pills with fewer side effects. But for now, eye drops remain the backbone of treatment.
The best choice isn’t the one with the lowest pressure number. It’s the one you can use every day without fear, discomfort, or confusion. That’s the real measure of success.
Can prostaglandins change my eye color permanently?
Yes. Prostaglandin analogs like latanoprost and bimatoprost can cause permanent darkening of the iris, especially in people with light-colored eyes (hazel, green, blue). This happens slowly over months or years and affects about 5% to 10% of long-term users. The change is irreversible, even after stopping the medication. It’s not harmful, but it can be cosmetically noticeable.
Are beta blockers safe if I have asthma?
No. Beta blockers like timolol can trigger severe bronchospasm in people with asthma or COPD. Even though the drops go in your eye, some gets absorbed into your bloodstream and can narrow your airways. The FDA requires a black box warning for this risk. If you have respiratory issues, your doctor should avoid beta blockers and choose prostaglandins or other alternatives instead.
Why do I need to press my tear duct after putting in eye drops?
Pressing gently on the inner corner of your eye (near your nose) for about a minute after applying drops blocks the tear duct. This prevents the medicine from draining into your nasal passages and being absorbed into your bloodstream. It’s especially important with beta blockers to reduce the risk of systemic side effects like low heart rate or breathing trouble. It also helps the drop stay in your eye longer, making it more effective.
Can I use two different prostaglandins together?
No. Combining two prostaglandin analogs-like latanoprost and bimatoprost-can actually increase eye pressure instead of lowering it. This is a known risk, supported by clinical studies. Even though they work similarly, using both together doesn’t add benefit and may harm your vision. Always use only one prostaglandin at a time unless your doctor specifically advises otherwise.
Do preservative-free eye drops work better?
Preservative-free drops improve comfort and reduce dry eye symptoms, especially for long-term users. But they don’t lower eye pressure any better than preserved drops. The difference in pressure control is tiny-about 0.3 mmHg-and not clinically meaningful. The main benefit is less irritation and better eye surface health. They cost more and require daily disposal, so they’re usually recommended only if you have significant dry eye or irritation from preserved drops.
How long does it take for glaucoma drops to start working?
Prostaglandins usually start working within a few hours, but it takes about 2 weeks to reach full effect. Beta blockers like timolol begin lowering pressure within 1 to 2 hours, with peak effect around 2 hours after use. Most doctors wait 4 to 6 weeks before checking eye pressure again to see the full impact. Don’t assume the drops aren’t working if you don’t feel anything-they don’t cause immediate sensations like pain relief would.
Can I stop using glaucoma drops if my pressure seems normal?
Never stop without talking to your doctor. Glaucoma damages your vision slowly and silently. Even if your pressure looks normal, the disease can still be progressing. Stopping medication can cause pressure to rise again, leading to irreversible vision loss. Most people need to take these drops for life. Regular checkups are essential-even if you feel fine.

so i read this whole thing and now im convinced the government is using glaucoma drops to secretly alter our iris color so they can track us via facial recognition... also why do they charge extra for preservative-free? someone's making bank off our blindness lol
my mom’s been on latanoprost for 5 years and her lashes are *chef’s kiss* 😍 but she swears her eyes look like a cat’s now... honestly tho, if it keeps her sight, i’ll take the dramatic lashes. she says she feels like a glam model with glaucoma 💅
Anyone else notice how these ‘prostaglandins’ are just a marketing gimmick pushed by Big Pharma to sell more expensive drops? Beta-blockers have been around since the 70s-effective, cheap, and if you can’t handle the side effects, maybe you shouldn’t be alive to begin with. This modern obsession with ‘cosmetic comfort’ is pathetic.
Let’s be real-prostaglandins aren’t treatment, they’re performance art. You’re not managing glaucoma, you’re curating a tragic beauty pageant where your iris is the crown and your lashes are the tiara. And let’s not pretend the red eyes aren’t just a side effect-they’re a fashion statement you didn’t ask for but now must live with. The real tragedy? You’ll never be able to go back to being ‘normal’ again. Welcome to the new aesthetic of chronic illness.
So you're telling me I have to choose between looking like a goth anime character or having a heart attack? That's not a medical decision-that's a horror movie plot. And now I'm supposed to press my tear duct? Like I'm some kind of Victorian lady with a handkerchief? This is ridiculous.
Wow, you people are so naive. Did you even read the FDA black box warning? Beta blockers don't just 'affect your lungs'-they can kill you quietly while you sleep. And prostaglandins? They're basically chemical tattoos on your eyeballs. You're not treating glaucoma-you're signing up for a lifelong body modification with no refund policy. And don't get me started on how they charge $300 for a bottle that costs $2 to make. This system is rigged.
Preservative-free formulations demonstrate statistically insignificant IOP reduction (Δ = 0.29 mmHg; p=0.41) per meta-analysis (J Glaucoma 2021), rendering cost differential clinically unjustifiable. Moreover, BAK-induced ocular surface disease remains underdiagnosed in primary care cohorts-yet the therapeutic index of preserved agents remains superior in long-term adherence metrics. Your emotional discomfort does not constitute a clinical endpoint.
GUYS. I JUST FOUND OUT THAT IF YOU USE TWO PROSTAGLANDINS TOGETHER, YOU CAN ACTUALLY MAKE YOUR GLAUCOMA WORSE?? 😱 I’M SO GLAD I READ THIS BEFORE I ACCIDENTALLY KILLED MY EYES 😭🙏🙏🙏
Stop taking them. Your vision will be fine.