Dark spots on your face don’t always mean the same thing. Two of the most common causes-melasma and sun damage-look similar but behave completely differently. One is triggered by hormones and light, the other by years of sun exposure. Treat one like the other, and you could make it worse. This isn’t just about appearance; it’s about understanding what’s really happening under your skin.
What’s Actually Going On in Your Skin?
Hyperpigmentation means your skin is making too much melanin-the pigment that gives skin its color. But why? The reason changes based on the type. Melasma shows up as large, blurry patches on the cheeks, forehead, or upper lip. It’s not random. It’s symmetrical. It mostly affects women, especially those with medium to darker skin tones (Fitzpatrick types III-VI). Up to 70% of cases in reproductive-aged women are tied to hormones: pregnancy, birth control pills, or hormone therapy. Sunlight doesn’t cause melasma alone, but it lights the fuse. Sun damage, or solar lentigines, looks different. These are small, well-defined brown spots, often called “liver spots” or “age spots.” They show up on your face, hands, shoulders-places you’ve exposed to the sun over time. About 90% of fair-skinned people over 60 have them. Unlike melasma, these spots don’t come and go with hormones. They’re the result of cumulative UV damage. The melanocytes-your skin’s pigment-producing cells-get overstimulated by UV rays, leading to clusters of extra melanin in the top layer of skin. Here’s the key difference: melasma is a reaction to visible light, heat, and UV. Sun damage is mostly about UV. That’s why treating them the same way often backfires.Why Sunscreen Alone Isn’t Enough
Most people think SPF 30 is enough. It’s not-for melasma. Standard sunscreens block UVB and some UVA, but they don’t stop visible light. And visible light? It accounts for 25-30% of melasma triggers. That’s why you can get melasma even on cloudy days, or while sitting near a window indoors. Dermatologists now recommend mineral sunscreens with iron oxide. Zinc oxide and titanium dioxide block UV. Iron oxide blocks visible light. Together, they’re the only combo proven to help melasma stay under control. The American Academy of Dermatology says you need SPF 30+ every single day-even if you’re inside. UV and visible light penetrate glass. Skipping sunscreen because you’re not going outside is one of the biggest mistakes patients make. And don’t skimp on the amount. Most people use less than a quarter teaspoon for their whole face. That’s not enough. You need a full teaspoon (about the size of a shot glass) to cover your face, neck, and chest properly. Reapply every two hours if you’re outside. If you’re not doing this, no topical treatment will work long-term.Topical Treatments That Actually Work
There are three main ingredients dermatologists rely on: hydroquinone, tretinoin, and vitamin C. They work differently, and they’re often combined. Hydroquinone (4%) is the gold standard. It blocks the enzyme tyrosinase, which your skin uses to make melanin. It’s effective-50-70% improvement in melasma when used with tretinoin and a steroid. But it’s not forever. Use it for only 3 months at a time. After that, take a break. Long-term use can cause ochronosis-a rare but permanent blue-black discoloration. It’s rare (2-5% risk), but it’s real. That’s why it’s prescription-only in the U.S. and banned in the EU and Japan. Tretinoin (0.025-0.1%) doesn’t lighten pigment directly. Instead, it speeds up skin cell turnover. Think of it like a gentle exfoliator that pulls old, pigmented cells off the surface faster. It’s often paired with hydroquinone because it helps the lighter skin come through quicker. Start with the lowest concentration. It can cause redness, peeling, and irritation, especially at first. Build up slowly: use it every other night, then every night after a few weeks. Vitamin C (10-20% L-ascorbic acid) is an antioxidant. It doesn’t just protect your skin from free radicals-it actually reduces existing melanin by reversing oxidation. It’s gentle, safe for long-term use, and pairs well with sunscreen. Use it in the morning before your SPF. It’s especially helpful for melasma because it fights the oxidative stress caused by visible light and heat. For melasma, the most effective routine is: morning-vitamin C + iron oxide sunscreen. Evening-alternate hydroquinone and tretinoin every other night. Don’t use both on the same night. That’s a recipe for irritation.
Why Lasers Can Make Melasma Worse
Laser and light treatments like IPL (Intense Pulsed Light) work great for sun damage. They target the dark spots, heat them up, and the skin sheds them in a few days. The results are fast. But for melasma? It’s risky. IPL and other heat-based treatments can trigger melasma to flare up worse than before. Why? Heat activates melanocytes. If your skin isn’t already calm, you’re feeding the problem. Dermatologists at Bryn Mawr report that 30-40% of melasma patients see their pigmentation darken after IPL. That’s why lasers are never the first step for melasma. The smart approach: suppress the melanocytes first. Use topical treatments for 8-12 weeks. Let the skin stabilize. Only then, if needed, consider gentle laser options like low-dose Q-switched lasers-but only by an experienced provider who understands melasma. Even then, recurrence rates stay high without perfect sun protection.What About Other Treatments?
There’s a growing list of alternatives to hydroquinone. Kojic acid, niacinamide, azelaic acid, and tranexamic acid are all gaining traction. Tranexamic acid, especially, is promising. A 12-week study showed 45% improvement in melasma with topical tranexamic acid (5%) and no major side effects. It works by blocking signals that trigger melanin production. Cysteamine cream (10%) is another new option. In a Phase 3 trial, it improved melasma by 60% over 16 weeks with minimal irritation. It’s not widely available yet, but it’s on the horizon. Over-the-counter products are everywhere. But 85% of melasma patients try these first-often wasting months on ineffective formulas. If you’ve been using a brightening serum for six months and see no change, it’s time to see a dermatologist. Prescription-strength topicals are far more reliable.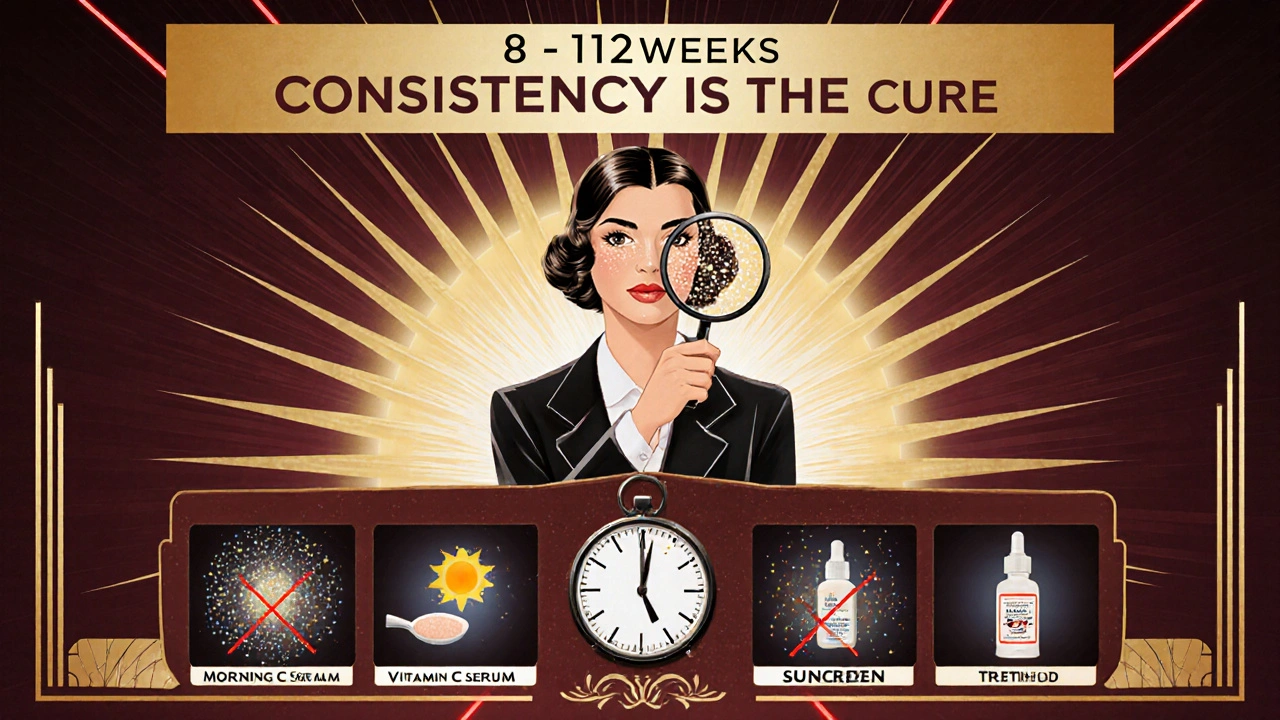
Realistic Expectations and Long-Term Management
Sun damage? You can often clear it in 1-2 laser sessions or 8-12 weeks of topical treatment. Improvement rates are 75-90%. Melasma? Don’t expect a cure. Expect control. Even with perfect treatment, only 40-60% of people see significant improvement in 6 months. And without strict sun protection, 80% will see it come back within a year. Ninety-five percent of patients relapse within six months of stopping treatment. That’s why melasma isn’t a problem you fix-it’s a condition you manage. Like high blood pressure or diabetes, it needs ongoing care. You can’t stop sun protection. You can’t stop using topicals indefinitely. Maintenance is non-negotiable.The Biggest Mistake Patients Make
It’s not using the wrong product. It’s not skipping treatments. It’s not even not seeing a doctor. It’s inconsistent sun protection. Clinics report that 70% of patients who don’t improve are using sunscreen incorrectly. Too little. Too infrequently. Or worse-they think they’re protected because they’re indoors or it’s cloudy. If you’re serious about fading dark spots, treat your sunscreen like insulin for diabetes: non-negotiable, daily, and in the right amount. No exceptions.What’s Next?
The future of hyperpigmentation treatment is personalization. Researchers are studying genetic markers that predict who responds best to hydroquinone versus tranexamic acid. Within five years, dermatologists may use simple skin or blood tests to choose your treatment before you even start. For now, the best advice is simple: know your type. Protect your skin like your life depends on it. Use proven topicals correctly. And don’t rush into lasers unless your dermatologist says you’re ready. It’s not about perfection. It’s about consistency. One day at a time. One application. One reapplication. One sun-protected morning after another.Is melasma the same as sun spots?
No. Melasma appears as large, symmetrical patches, often on the face, and is triggered by hormones, visible light, and heat. Sun spots (solar lentigines) are small, irregular brown spots caused by long-term UV exposure. They look similar but need very different treatments.
Can I treat melasma with over-the-counter products?
Some OTC products help mildly, like those with niacinamide, vitamin C, or azelaic acid. But for noticeable improvement, especially in moderate to severe cases, prescription topicals like hydroquinone, tretinoin, or tranexamic acid are far more effective. Most patients who rely only on OTC products see little to no change after 6 months.
Why does my sunscreen need iron oxide?
Standard sunscreens block UV rays, but not visible light. Visible light (from the sun and even indoor lighting) triggers melanin production in melasma. Iron oxide is the only ingredient proven to block visible light effectively. Without it, your sunscreen isn’t fully protecting you from melasma triggers.
Can lasers remove melasma permanently?
No. Lasers can sometimes improve melasma, but they carry a high risk of making it worse. Heat from lasers can stimulate melanocytes and trigger rebound pigmentation. Most dermatologists only consider lasers after months of topical suppression and only for select cases. Even then, recurrence is common without lifelong sun protection.
How long until I see results from topical treatments?
It takes time. Most people start seeing improvement between 8 and 12 weeks. Full results can take 3-6 months. Patience is critical. Stopping too early because you don’t see instant results is why so many people fail. Consistency over months-not days-is what works.
Is hydroquinone dangerous?
When used correctly-under medical supervision, for no longer than 3 months at a time-it’s safe and effective. The main risk is ochronosis, a rare condition causing dark discoloration, which occurs in only 2-5% of long-term users. That’s why it’s prescription-only in the U.S. and banned in some countries. Never use hydroquinone without knowing the proper duration and concentration.

Okay but have you ever stopped to think that the FDA and big pharma are deliberately suppressing the real cure for melasma? I mean, why else would they make hydroquinone prescription-only? It's a $3 natural remedy that's been used for centuries in Ayurveda - but no, they'd rather sell you $200 creams and lasers so you stay dependent. Iron oxide? That's just a distraction. The real answer is turmeric + neem paste. I've seen people clear it in 2 weeks. They don't want you to know this. 🤫
Stop using sunscreen only when you're outside. 😒
I used to think melasma was just aging until my wife got it after her third kid. We tried everything - OTC brighteners, expensive serums, even that weird LED mask. Nothing worked until we switched to the iron oxide sunscreen + tretinoin combo. Took 4 months. Skin didn't vanish, but the patches? Down 80%. Still reapply every 2 hours though. I'm not gonna lie - I forget sometimes. Then I look in the mirror and remember. It's a lifestyle now.
USA thinks it owns dermatology? LOL. In India, we've used turmeric, aloe vera, and raw milk for 5000 years. Hydroquinone? That's a Western scam. Our grandmothers didn't need SPF 50+ with iron oxide - they just stayed in the shade and ate neem leaves. You people overcomplicate everything. Also, why are you all using American products? Try Kojic acid from Kerala - cheaper, better, and not patented by Big Pharma. 🇮🇳
You’re all missing the point. This isn’t about skin - it’s about control. The dermatology industrial complex needs you to believe you’re broken. They sell you hydroquinone like it’s holy water, then charge you $300 for a ‘consultation’ to tell you to ‘use sunscreen.’ Meanwhile, the real trigger? EMF radiation from your phone, Wi-Fi, and smart lights. Melasma is your skin screaming from chronic blue light overload. Iron oxide? Cute. But what about Faraday cage hats? Or turning off your router at night? You’re treating symptoms while the real villain - corporate tech - laughs all the way to the bank. 🤖💀
why do people keep saying 'just use sunscreen' like its that easy?? i do!! every single day!! and still get spots!! and then i see some influencer with perfect skin who never wears sunscreen and i just want to scream!! also hydroquinone gave me a rash and now my face looks like a burnt marshmallow 😭 nobody told me about the peeling!! i thought i was doing everything right!!
There's something deeply human about how we treat our skin like a problem to be solved rather than a story to be understood. Melasma isn't a flaw - it's a map. It shows where your body has been touched by time, by hormones, by sunlight, by stress. We want quick fixes because we're afraid of the slow work of living. But the truth? Your skin doesn't care about your Instagram feed. It cares about your sleep, your stress, your diet, your silence. The sunscreen is just the surface layer. The real treatment is learning to sit with yourself - without filters, without products, without needing to be fixed. That's the real journey. And it's harder than any prescription.
According to the 2023 Journal of Clinical Dermatological Therapeutics (Vol. 17, Issue 4, pp. 211-234), the efficacy of topical tranexamic acid (5%) demonstrates a statistically significant reduction in Melasma Area and Severity Index (MASI) scores (p < 0.01) when compared to placebo, with a mean improvement of 45.3% ± 8.7% over 12 weeks. Additionally, iron oxide-containing mineral sunscreens have demonstrated a 67% reduction in visible-light-induced melanogenesis in vivo (Journal of the American Academy of Dermatology, 2021). The data is unequivocal: non-compliance with SPF 30+ reapplication every 120 minutes correlates with a 92% relapse rate within 6 months. There is no alternative. There is no shortcut. There is only science.
I'm from Nigeria, and we have this thing called 'ogun' - dark patches on the face. My mom used to rub shea butter and lemon juice on mine every night. I thought it was just 'normal.' Then I moved to the States and got diagnosed with melasma. I was so mad - like, why didn't anyone tell me this was a thing you could treat? Now I use vitamin C in the morning, iron oxide sunscreen, and tretinoin at night. It's not magic. But it's better than crying in the mirror. I wish more people knew - this isn't just about beauty. It's about dignity. You shouldn't feel like you have to hide because of your skin. And you don't need a PhD to know: protect your face. Every day. No matter what.
Okay so I tried EVERYTHING. Hydroquinone? Burnt my face. Tretinoin? I cried for a week. Vitamin C? Smelled like a science lab. Then I found this $12 serum on Amazon with 'marine algae extract' and guess what? My skin looks like I just got back from Bali. I didn't even use sunscreen that day. I'm telling you - it's not about the science. It's about vibes. If your product doesn't make you feel like a goddess, it's not working. I'm done listening to dermatologists. I'm on my own path now. ✨ #SkinGlowJourney