Switching from a brand-name drug to a generic version is supposed to save money-without sacrificing effectiveness. For most people, it works just fine. But for some, a simple change in pill color or shape can trigger headaches, anxiety, seizures, or even hospitalization. If you’ve noticed something off after your pharmacy switched your medication, you’re not imagining it. And you’re not alone.
Why Switching Generics Can Cause Problems
Generic drugs are required by the FDA to have the same active ingredient as the brand-name version. That part is true. But what’s not always said is that generics can differ in their inactive ingredients-fillers, dyes, coatings, and how the drug is released in your body. These differences are usually harmless. But for certain medications, even tiny changes can throw off your treatment. The FDA allows generics to absorb 80% to 125% as much of the drug as the brand-name version. That means two different generics of the same drug could vary by up to 45% in how much enters your bloodstream. For most drugs, that’s fine. But for drugs with a narrow therapeutic index-where the difference between a helpful dose and a dangerous one is small-those variations matter. These are the drugs where switching causes the most trouble:- Antiepileptics like divalproex sodium and phenytoin
- Thyroid meds like levothyroxine
- Anticoagulants like warfarin
- Immunosuppressants like tacrolimus
- Extended-release ADHD meds like Adderall XR and bupropion XL
A 2019 study in BMJ Open found that patients switching between generic versions of heart meds had a 12.3% higher risk of being hospitalized within 30 days. For people with epilepsy, a 2021 survey of neurologists showed that nearly 7 out of 10 believed switching generics increased seizure risk. And in one hospital study, 20% of patients who accidentally got duplicate prescriptions after multiple switches ended up with serious side effects-including one case of serotonin syndrome.
Real People, Real Side Effects
You won’t find these stories in FDA brochures. But you’ll find them on Reddit, in patient forums, and in doctors’ offices. One man on r/ADHD wrote: “I switched from brand Adderall to a generic. Within 24 hours, I couldn’t focus, felt like I was in a fog, and my heart was racing. I thought I was having a panic attack. Turns out, it was the new generic.” He got his old version back after his doctor intervened. Another patient switching from brand levothyroxine to a generic reported fatigue, weight gain, and brain fog-symptoms she hadn’t had in years. Her TSH levels jumped from 2.1 to 7.8 after the switch. Her doctor had to re-prescribe the original brand. A MedShadow survey of over 1,200 people taking generic ADHD meds found that 63% noticed reduced effectiveness after a manufacturer switch. Over 40% reported new side effects: headaches (28%), anxiety (22%), and stomach issues (19%). These aren’t rare outliers. They’re common enough that neurologists, pharmacists, and psychiatrists are starting to take notice.Why This Keeps Happening
The problem isn’t just bad drugs. It’s the system. Pharmacy benefit managers (PBMs)-companies like CVS Caremark and Express Scripts-control which generics pharmacies stock. They don’t care about your stability. They care about rebates. Every time a drugmaker offers a bigger discount, the PBM switches the preferred generic. That means you might get one brand this month, a different one next month, and another the month after that. According to Senate committee data, PBMs change preferred generic manufacturers an average of 4.7 times per year per drug. For someone on a chronic medication, that’s nearly five switches a year. And most patients don’t even know it’s happening. Levothyroxine alone has 12 FDA-approved generic manufacturers. Each uses different binders and coatings. One might release the drug slowly. Another might release it fast. Your body doesn’t care about the label-it cares about what’s inside and how it gets there.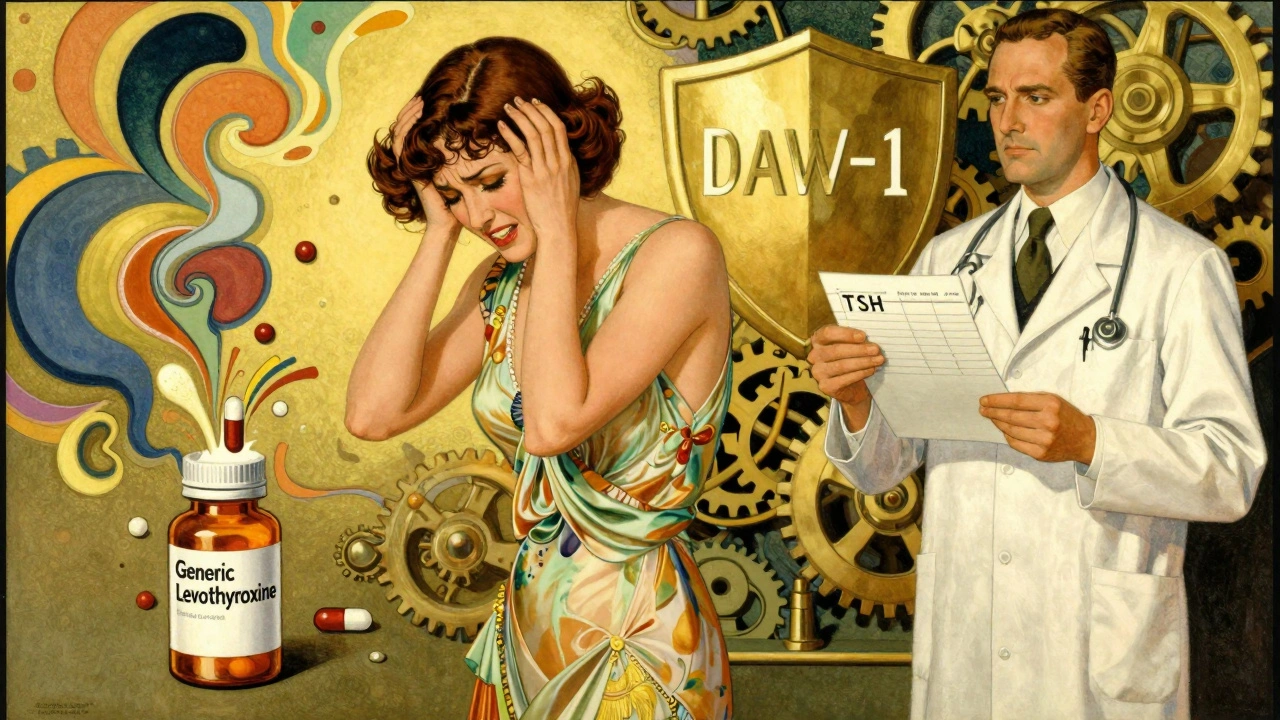
When to Worry: Red Flags After a Switch
Not every change means trouble. But if you notice any of these within 72 hours of a new prescription, pay attention:- New or worsening anxiety, depression, or mood swings
- Sudden return of symptoms (seizures, chest pain, fatigue, brain fog)
- Unexplained headaches, nausea, or dizziness
- Heart palpitations or unusual fatigue
- Changes in sleep, appetite, or weight
These aren’t just “side effects.” They could be signs your body isn’t getting the right dose. For thyroid patients, even a small change in levothyroxine absorption can send TSH levels soaring. For epilepsy patients, a 10% drop in drug levels can trigger a seizure.
What You Can Do
You don’t have to accept this. Here’s how to protect yourself:- Ask for the manufacturer name. When you pick up your prescription, ask: “Which company made this?” Write it down. If your pill looks different from last time, ask why.
- Check the NDC code. It’s a 10-digit number on the bottle. If it changes, the manufacturer changed. Keep a log. Apps like Medisafe or MyTherapy can help.
- Request “dispense as written.” Ask your doctor to write “DAW-1” on your prescription. That tells the pharmacy not to substitute. This is especially important for NTI drugs.
- Get lab tests if needed. For thyroid, warfarin, or epilepsy meds, ask your doctor to check levels 2-4 weeks after a switch. A simple blood test can tell you if the new version is working.
- Talk to your pharmacist. Pharmacists can often order your preferred generic if it’s available. Many will do it if you ask.
A 2021 study showed patients who got counseling from a pharmacist about switching risks were 37% less likely to have problems. That’s not magic. It’s awareness.
What’s Changing-And What’s Not
There’s some good news. In 2023, Medicare Part D started limiting generic switches to no more than twice a year. The FDA launched a new initiative to improve testing for complex generics like inhalers and extended-release pills. And in January 2024, the American Society of Health-System Pharmacists updated its guidelines to recommend against automatic substitution for 17 high-risk drugs, including tacrolimus and bupropion XL. But the system still favors cost over consistency. PBMs still push switches for rebates. Pharmacies still fill the cheapest option unless told otherwise.The Bottom Line
Generics save billions. That’s important. But not at the cost of your health. If you’re on a medication for epilepsy, thyroid disease, heart conditions, or mental health-and you’ve noticed something off after a refill-it’s not in your head. It’s real. And you have the right to ask for stability. Don’t wait for a crisis. Talk to your doctor. Track your pills. Know your NDC code. And if you feel worse after a switch, speak up. Your body is telling you something. Listen.Can generic drugs really be less effective than brand-name ones?
Yes, for certain medications. While generics must meet FDA bioequivalence standards, those standards allow up to a 20% difference in how the drug is absorbed. For drugs with a narrow therapeutic index-like levothyroxine, warfarin, or antiepileptics-even small changes can lead to treatment failure or side effects. Studies show patients switching between generic versions of these drugs have higher rates of hospitalization and symptom recurrence.
Which generic drugs are most likely to cause problems after a switch?
The highest-risk drugs include antiepileptics (phenytoin, divalproex), thyroid medications (levothyroxine), blood thinners (warfarin), immunosuppressants (tacrolimus), and extended-release psychiatric drugs (Adderall XR, bupropion XL). These drugs have tight safety margins, and minor differences in how they’re made can affect how your body responds.
Why do pharmacies switch my generic medication so often?
Pharmacy benefit managers (PBMs) like CVS Caremark and Express Scripts control which generics are stocked. They choose based on rebates-discounts drugmakers pay to get their product on the preferred list. The highest bidder wins, even if it means switching you to a different manufacturer every few weeks. This happens an average of 4.7 times a year per drug.
How can I find out which company made my generic drug?
Look at the NDC code on your prescription bottle-it’s a 10-digit number. You can enter it into the FDA’s National Drug Code Directory online to find the manufacturer. You can also ask your pharmacist directly. Many will tell you if you ask. Keep a record of the manufacturer and pill appearance for future reference.
Can I ask my doctor to prevent generic switches?
Yes. Ask your doctor to write “DAW-1” (Dispense As Written) on your prescription. This legally prevents the pharmacy from substituting a different generic without your consent. This is especially important for high-risk medications. Some doctors are hesitant, but if you explain your concerns and have documentation of side effects, most will comply.
Should I avoid generics altogether?
No. For most people and most medications, generics are safe and effective. The problem isn’t generics-it’s frequent, unmonitored switching between different manufacturers. If you’re on a stable dose of a low-risk drug like a statin or an antibiotic, switching is usually fine. But for high-risk medications, consistency matters. Work with your doctor to find the right balance between cost and safety.
What should I do if I think a generic switch caused side effects?
First, don’t stop taking your medication without talking to your doctor. Then, document everything: when you switched, what the pill looked like, what symptoms started, and when. Contact your pharmacist to find out which manufacturer made your last refill. Schedule a follow-up with your doctor to check blood levels if applicable. Request your previous generic or brand-name version if it worked better. Your experience matters-and you have the right to be heard.

So let me get this straight - we’re paying billions to drug companies so they can sell us the same pill with a different color and call it a ‘generic’? And the FDA’s like ‘eh, 20% variance is chill’? Bro. My thyroid meds switched manufacturers last month and I felt like a zombie who forgot how to breathe. Now I’m logging NDC codes like it’s my job. 🤡
Y’all are NOT alone!! 💪 I switched generics for my levothyroxine and went from feeling amazing to crying in the shower for no reason. My doctor didn’t believe me until my TSH jumped to 8.2. Now I ask for the brand name every time - and I tell them I’ll pay extra. My health > their profits. You got this!! 🌞
It’s not the generic. It’s the system. PBMs are corporate vampires. They don’t care if you seizure or die. They care about the rebate check. You think this is an accident? Nah. It’s designed. They want you unstable so you’ll keep coming back. Profit over people. Always.
Thank you for writing this. 🙏 I’ve been terrified to speak up because people think I’m ‘overreacting’ - but my anxiety went from manageable to panic attacks daily after a switch. I finally asked for DAW-1 and my life changed. You’re not crazy. You’re just paying attention. Keep going. We’re rooting for you. ❤️
I’m a nurse and I see this every week. Patients come in saying ‘I don’t know why I feel awful’ - and it’s always a new generic. We don’t get training on this stuff. But we should. Doctors don’t always know either. Just asking for the manufacturer name can save someone’s life.
THIS IS A GOVERNMENT COVER-UP. The FDA, Big Pharma, and PBMs are all in cahoots. They want you dependent. They want you confused. They want you taking 3 different generics a year so you keep buying more pills. They’re poisoning us with ‘inactive ingredients’ - that’s just code for ‘we added chemicals to make you sick so you’ll need more drugs.’ Wake up. The NDC code is your only weapon.
In India, generics are the only option and most work fine. But I see your point - if the release profile changes, it matters. Especially for epilepsy and thyroid. My cousin had seizures after switching. He went back to the original and was fine. It’s not about country - it’s about consistency.
Let’s be real - this isn’t about healthcare. It’s about control. The system doesn’t want you stable. It wants you revolving. Every switch is a psychological reset. Your body doesn’t just react to the drug - it reacts to the *uncertainty*. That’s why anxiety spikes. That’s why brain fog returns. They’re not just changing pills. They’re changing your reality. And you’re supposed to be grateful for the discount.
I had the same thing with Adderall. Switched generics, felt like I was underwater. Took me 3 weeks to figure out it wasn’t me - it was the pill. I started taking a photo of every bottle before I take it. Now I know when it changes. My doctor finally listened after I showed him the photos. You’re not weak. You’re just observant.
My mom’s on warfarin. Last month, her INR spiked to 5.2 after a ‘routine’ generic switch. She almost bled out. Turns out, the new version released the drug 40% faster. The pharmacist said ‘it’s the same drug.’ I said ‘then why did she almost die?’ They didn’t have an answer. Now we track everything. No more blind faith.