It’s easy to think that if you’re taking medications as prescribed, you’re safe. But what if one of your pills is quietly messing with another? A drug interaction doesn’t always come with a warning label. Sometimes, it starts with a weird feeling - a racing heart, a rash that won’t go away, or sudden dizziness you can’t explain. And if you ignore it, what seems like a minor glitch could turn into a life-threatening emergency.
What Counts as a Dangerous Drug Interaction?
A drug interaction happens when one substance changes how another works in your body. This could be a prescription, an over-the-counter pill, a supplement, even food or alcohol. The most serious ones happen between two or more drugs that affect the same system - like your heart, liver, or brain. The FDA says these interactions can make a drug less effective, cause unexpected side effects, or make it too strong. That last one is the real danger. For example, mixing warfarin (a blood thinner) with certain antibiotics can turn a small cut into a dangerous bleed. Or combining SSRIs like sertraline with painkillers like tramadol can trigger serotonin syndrome - a condition where your brain gets flooded with too much serotonin. Symptoms start mild but can spiral fast. Temperature spikes, muscles lock up, your heart races. Without quick help, it can be fatal.Call 911 Right Now If You Have These Symptoms
Some reactions don’t wait. If you’re experiencing any of these, don’t call your doctor - don’t wait to see if it gets better. Get help immediately.- Difficulty breathing or oxygen levels below 90% - This isn’t just feeling winded. If you’re gasping, your lips are turning blue, or you have a pulse oximeter reading under 90%, your airway or lungs are in trouble.
- Swelling of the face, lips, tongue, or throat - Angioedema can block your airway in minutes. Even if it starts small, it can worsen fast. Don’t wait to see a doctor. Go to the ER.
- Systolic blood pressure below 90 with a heart rate over 120 - This is shock territory. Your body is failing to circulate blood. It’s not just feeling lightheaded. You might feel cold, clammy, or confused.
- Seizures lasting more than 2 minutes - Especially if you’re on medications like lidocaine, certain antibiotics, or antipsychotics. A seizure is not normal after taking a pill. Call 911.
- Temperature above 41.1°C (106°F) with rigid muscles and extreme agitation - This is serotonin syndrome at its worst. Muscles lock, you sweat uncontrollably, and your mind races. It’s rare but deadly if untreated.
These aren’t "maybe" symptoms. They’re red flags that mean your body is in crisis. Delaying care increases your risk of organ damage or death.
See a Doctor Within 24 Hours If You Notice These Signs
Not every bad reaction needs an ambulance. But if you’ve started a new medication or changed a dose, and you’re feeling off, don’t brush it off. Some reactions build slowly but still need urgent attention.- A rash covering more than 30% of your skin - Not just a little red spot. If it’s widespread, itchy, and spreading, it could be DRESS syndrome - a severe immune reaction linked to anticonvulsants, antibiotics, or allopurinol.
- Unexplained fever over 38.5°C (101.3°F) for more than 48 hours - Especially if you’re on antibiotics, antivirals, or seizure meds. This isn’t a cold. It could be serum sickness or another systemic reaction.
- Unusual bruising, bleeding gums, or nosebleeds - If your platelet count drops below 100,000/μL, you’re at risk for internal bleeding. Some antibiotics, diuretics, and even herbal supplements like ginkgo can cause this.
- Yellow skin or eyes, dark urine, or right-side abdominal pain - These point to liver damage. ALT levels above 120 U/L mean your liver is stressed. Drug-induced liver injury is silent until it’s advanced.
- Urinating less than half a cup every 2 hours for 6+ hours - Plus rising creatinine. This is kidney trouble. Many painkillers, blood pressure meds, and antibiotics can harm the kidneys over time.
These symptoms don’t always mean you’ve had a bad reaction. But if they show up after starting a new drug, they’re a signal. Your doctor needs to check your blood, adjust your meds, or switch you to something safer.
What Makes Some Interactions More Dangerous Than Others?
Not all drugs are created equal. Some have a "narrow therapeutic index" - meaning the difference between a helpful dose and a toxic one is tiny. Even a small change in how your body processes the drug can be deadly. Drugs like warfarin, digoxin, phenytoin, and lithium fall into this category. A common antibiotic like amoxicillin can raise warfarin levels by 20%. That might sound small, but for someone on warfarin, that’s enough to cause a stroke or internal bleeding. That’s why experts like Dr. David Juurlink from Sunnybrook Hospital say: "If you’re on one of these drugs, treat every new medication - even a cough syrup - as a potential threat." Always check with your pharmacist before adding anything new.
Why People Wait Too Long - And What Happens When They Do
Most people don’t realize they’re having a drug interaction. They think, "I’m just tired," or "My stomach is upset because I ate something bad." A 2023 survey on MedHelp found that 72% of people who later confirmed a drug interaction had ignored early symptoms for over 12 hours. The National Community Pharmacists Association found that 58% of patients waited more than half a day before calling their doctor - even after experiencing dizziness, nausea, or confusion. By then, the reaction was often worse. On the flip side, those who acted fast had better outcomes. According to the American Association of Poison Control Centers, 89% of people who called poison control within an hour of noticing symptoms avoided the ER entirely. Poison control centers are trained to spot these patterns. They can tell you whether it’s safe to wait, or if you need to go in.How to Prevent Drug Interactions Before They Start
Prevention beats reaction every time. Here’s how to protect yourself:- Keep a complete list of everything you take - Not just prescriptions. Include vitamins, herbal supplements (like St. John’s wort or turmeric), over-the-counter painkillers, and even recreational substances like alcohol or cannabis. One in five serious interactions involves a supplement.
- Use a reliable drug interaction checker - Drugs.com has a free tool that checks over 24,000 medications. But make sure you enter everything. Missing one item can give you false confidence.
- Ask your pharmacist every time - They’re the most accessible experts. When you pick up a new script, ask: "Could this interact with anything else I’m taking?" Most pharmacists will run the check for free.
- Use the STOP method - If you suspect an interaction: Stop the new medication, Telephone your provider, Observe your symptoms, Present all your medication containers at your appointment.
Health systems are getting better at warning doctors. The 21st Century Cures Act requires electronic health records to flag interactions. But studies show 47% of doctors ignore alerts because they get too many false alarms. That’s why you can’t rely on the system alone. You need to be your own advocate.
What to Do If You’re on 5 or More Medications
If you’re taking five or more drugs - which affects nearly half of adults over 65 - your risk of a major interaction jumps to 57%. That’s not a small chance. That’s a high-stakes game. Talk to your doctor about a "medication review." This isn’t just checking if you’re taking them right. It’s asking: "Do I still need all of these?" Many older adults are on drugs prescribed years ago for conditions that no longer exist. Cutting back can reduce your risk without losing benefits. Use a pill organizer with alarms. Keep a written log of side effects. Bring your list to every appointment - even if you’ve seen the doctor before. Changes happen fast. A new antibiotic, a different blood pressure pill, a new supplement - each one could shift your balance.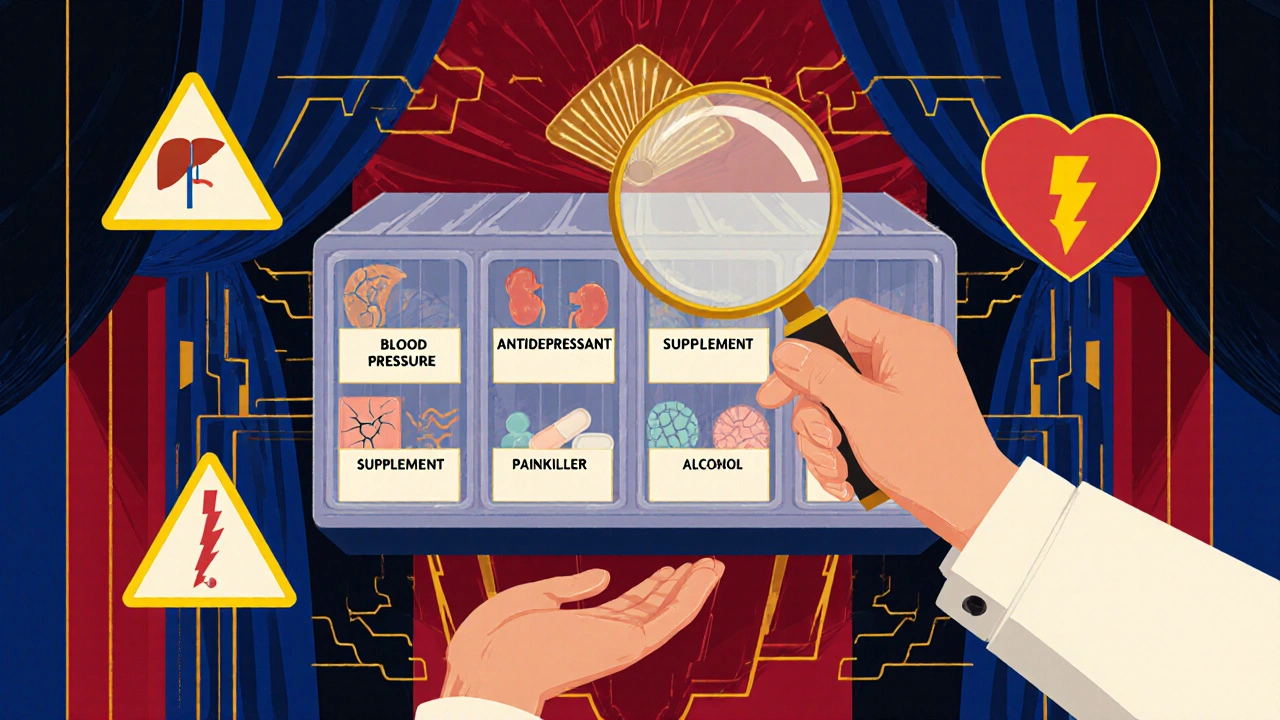
What’s Coming Next
Technology is catching up. AI tools like IBM Watson Drug Insights can predict new interactions before they’re even documented. The FDA is expanding its real-world data network to track 300 million patient records, looking for hidden patterns. By 2025, new rules will require drug makers to report interactions found in real patients - not just lab studies. But none of that helps you today if you’re sitting at home, wondering if your headache is just stress - or a sign your liver is failing.Frequently Asked Questions
Can over-the-counter meds cause dangerous drug interactions?
Yes. Common painkillers like ibuprofen or naproxen can interfere with blood pressure meds, increase bleeding risk with warfarin, or harm the kidneys when taken with diuretics. Even antacids like omeprazole can reduce the absorption of certain antibiotics or antifungals. Don’t assume "over-the-counter" means "safe to mix."
Are herbal supplements safe to take with prescription drugs?
No, not without checking. St. John’s wort can cut the effectiveness of birth control, antidepressants, and HIV meds. Garlic and ginkgo can thin your blood, raising bleeding risk during surgery or with warfarin. Turmeric may interfere with chemotherapy. Supplements aren’t regulated like drugs, so their strength and interactions are unpredictable.
How long after taking a new drug do interaction symptoms usually appear?
It varies. Some reactions happen within hours - like an allergic rash or sudden dizziness. Others, like liver or kidney damage, can take days or weeks to show up. That’s why it’s important to monitor yourself closely for at least two weeks after starting a new medication.
Can alcohol interact with my medications?
Absolutely. Alcohol can intensify drowsiness from sedatives, increase liver damage from painkillers like acetaminophen, and raise blood pressure when mixed with antidepressants. Even moderate drinking can turn a safe dose into a dangerous one. Always ask if alcohol is safe with your meds.
What should I bring to the ER if I suspect a drug interaction?
Bring all your medications - pills, patches, liquids, even empty bottles. Include supplements, vitamins, and herbal products. If you have a list of what you took and when, bring that too. This helps doctors identify the culprit faster. Don’t rely on memory - you may be too sick to recall everything.
Can I call poison control instead of going to the ER?
Yes - and you should. Poison control centers are staffed 24/7 by pharmacists and nurses trained in drug reactions. They can help you decide if you need to go to the hospital, if you can wait, or if you need to take an antidote. In 65% of cases, they manage the issue without hospital visits. Save the number in your phone: 1-800-222-1222 (U.S.) or your local poison center.

Just started a new blood pressure med last week and got this weird fluttery feeling in my chest. Thought it was anxiety but then I read this and freaked out. Called my pharmacist right away and they said it could be interacting with my fish oil. Switched me to a different brand and boom - gone. Don't ignore those little weird vibes, y'all. Your body's trying to talk to you.
Also, PLEASE keep a list of everything you take. I used to just remember the big pills. Turns out my gummy vitamins had potassium in them and that was part of the problem. Life-changing habit.
LMAO so now we're treating every little headache like a biohazard? 😂
My grandma took 17 pills a day and lived to 92. She didn't have a 'medication review' - she had a bottle labeled 'Mystery Mix' and a bottle of whiskey. She's still alive. You're telling me I can't take Tylenol with my antidepressants? Bro. I've been doing it for 8 years. Nothing happened. Until now. Now I'm a walking medical liability.
Also, poison control? I'd rather swallow a bee than call some stranger who sounds like they're reading from a script. 🤡
It is imperative to underscore the profound public health significance of this subject. The prevalence of polypharmacy among elderly populations, coupled with inadequate patient education regarding pharmacokinetic and pharmacodynamic interactions, constitutes a critical vulnerability within our current healthcare infrastructure.
While electronic health record alerts are theoretically robust, their clinical utility is severely diminished by alert fatigue, a well-documented phenomenon in the literature. Consequently, patient empowerment through diligent self-advocacy - including the maintenance of an accurate, up-to-date medication inventory and proactive consultation with licensed pharmacists - remains the most reliable safeguard against iatrogenic harm.
I commend the author for this comprehensive and evidence-based exposition. Such clarity is desperately needed in an era where misinformation proliferates faster than clinical guidelines can be updated.
I keep thinking about how we’ve turned medicine into this high-stakes game of Jenga where every new pill is another block. And we’re all just standing there, hoping the tower doesn’t fall.
Why is it that we’re so good at warning people about eating too much sugar or smoking, but when it comes to mixing pills? We just shrug and say 'oh, it’s fine.'
My mom took a new antibiotic and got this weird skin rash. She thought it was laundry detergent. Took three days to get to the doctor. Turns out it was DRESS syndrome. She was in the hospital for two weeks.
It’s not about being paranoid. It’s about being aware. We’re taught to trust doctors, but we’re not taught to ask the right questions. Like - 'What happens if I take this with my turmeric?'
And why do we think supplements are 'natural' so they’re safe? That’s like saying wild mushrooms are safe because they grow in the forest.
It’s weird how we live in this age of supercomputers and DNA sequencing, but we still treat our bodies like black boxes we don’t need to understand.
I wish we had a class in high school on this. Like, 'Medicines 101: Don’t Die Because You Didn’t Ask.'
Also, poison control is literally free and available 24/7. Why are we so afraid to call them? It’s not a judgment call. It’s a life-saving hotline.
Man, I love how this post just drops the truth like a bomb. I’ve been on 6 meds for years and never thought twice about my CBD oil. Then I got a weird dizzy spell and checked it. Turns out CBD can mess with my blood thinner. Scared the hell out of me.
Just called my pharmacist and she was super chill. Ran the check, said 'yeah, swap to a different brand or cut the dose.' No drama. Just science.
Also, I’m British but I live in Texas now - and I can’t believe how many people here think 'natural' means 'safe.' I’ve seen people take 10 different herbs with their heart meds. One guy was taking garlic pills and ginkgo and warfarin. He almost bled out during a tooth extraction.
So yeah - keep the list. Ask the pharmacist. Don’t be a hero. Your liver doesn’t care how 'well-informed' you think you are.
Okay but why are we acting like this is new info? Like, every drug commercial has that 10-minute disclaimer with a guy falling off a bike while eating grapefruit.
And why do we still think supplements are 'not real medicine'? I’ve seen people take 8 different 'natural' things and then act shocked when they get liver damage.
Also, poison control? Please. I called once and they asked if I was 'conscious.' Like, that’s the first question? I’m calling because I’m about to pass out, not to play 20 questions.
And don’t even get me started on doctors ignoring alerts. If your system is so broken that it gives you 200 fake warnings a day, maybe the system needs to change, not just you to 'be your own advocate.'
Also, why is everyone so obsessed with 'medication reviews'? Sounds like a corporate buzzword for 'we’re gonna try to take your pills away.'
Anyway, I still take melatonin with my antidepressants. And I’m fine. So maybe we’re all just scared of our own shadows.
Given the pharmacokinetic and pharmacodynamic profiles of commonly co-administered agents, the risk stratification for drug-drug interactions is not adequately addressed in primary care settings due to systemic under-resourcing and cognitive overload among prescribers.
Moreover, the absence of standardized pharmacogenomic screening protocols in outpatient environments renders population-level risk mitigation statistically untenable.
Furthermore, the proliferation of unregulated nutraceuticals - many of which exhibit CYP450 enzyme modulation - introduces a confounding variable that exceeds the diagnostic bandwidth of current clinical decision support systems.
Consequently, patient self-reporting remains the most unreliable data stream in the interaction risk assessment chain, as evidenced by 72% non-disclosure rates in retrospective surveys.
Therefore, a paradigm shift toward mandatory pharmacist-led medication reconciliation at every dispensing event is not merely prudent - it is ethically imperative.
Look, I get it. But let’s be real. America’s got the best doctors, the best hospitals, the best drugs. You want to know why people die from interactions? Because they’re too lazy to read the damn label.
My cousin took Adderall and drank energy drinks. Died. Wasn’t the drug’s fault. Was his. He thought 'it’s just caffeine.' No. It’s not. You don’t mix stimulants. That’s like driving with your foot on the gas and the brake.
And don’t even get me started on supplements. 'Oh, it’s natural!' Yeah, arsenic is natural too. Doesn’t mean you eat it.
Stop acting like this is some conspiracy. It’s basic common sense. If you don’t know what you’re taking, don’t take it. Simple. No magic. No AI. Just brains.
And if you’re on 5+ meds? You’re not a patient. You’re a walking pharmacy. Get your act together.
OMG this is so important!! 🙏😭 I just found out my magnesium supplement was messing with my thyroid med 😱 I thought it was just stress! Now I keep a little notebook and check everything on Drugs.com 📒💻
Also, poison control is my hero 💖 They helped me when I thought I was having a heart attack but it was just a weird reaction to a new antibiotic. They told me to drink water and wait. I did. No ER. Saved me $1200 💸
PS: I started putting all my meds in a clear bag and taking it to every appointment. It’s kinda embarrassing but so worth it 😅
so i took a new pain pill and got super dizzy and thought i was just dehydrated but then i read this and realized maybe it was the interaction with my blood pressure med?? i didnt know supplements could do that too?? like my gummy vitamins?? omg im so dumb.
called my doc and they said yep, thats a thing. switched me to a different one. no big deal. but i almost ignored it because i thought it was just 'me being tired.'
also why do we not teach this in school?? like at all??
I’ve been on 7 meds for 10 years. Never had an issue. I don’t use apps or lists. I just remember. I’m 71. I’ve survived worse.
My wife says I should check everything. I say, 'if it ain’t broke, don’t fix it.'
But then last week I started taking a new probiotic and got a rash. Didn’t think much of it. Two days later, my hand swelled up. Went to urgent care. Turns out the probiotic had a hidden ingredient that reacted with my statin.
So… maybe I’ll start writing things down. Not because I’m scared. Just because… well, I don’t want to end up like that guy on the news.
Also, I still don’t trust those online checkers. They always say 'possible interaction' when it’s probably nothing. But I’ll ask my pharmacist next time. He’s a good guy.
Thank you for sharing your experience, Alex. Your anecdote underscores the very principle this post advocates: vigilance, not fear. Even those with long-standing medication regimens are not immune to new variables - whether a new supplement, a change in diet, or even altered renal function due to aging.
The fact that you recognized the rash as unusual and sought care, despite your initial skepticism, is precisely the behavior we should encourage. It is not weakness to question. It is wisdom.
And yes - your pharmacist is not a gatekeeper. He is your ally. Treat him as such.