Sulfonylurea Safety Calculator
This tool calculates your risk of severe hypoglycemia when taking sulfonylurea medications. Based on clinical evidence from the article, it helps you understand which sulfonylurea might be safest for your specific situation.
Your Risk Factors
Risk Assessment
When you're managing type 2 diabetes, picking the right medication isn't just about lowering blood sugar-it's about staying safe. Among the oldest and cheapest oral diabetes drugs, sulfonylureas still get prescribed often, especially when cost matters. But not all sulfonylureas are the same. Some can send your blood sugar crashing so low you end up in the ER. Others? Much safer. The difference isn't subtle. It's life-changing.
Why Sulfonylureas Still Matter
Sulfonylureas have been around since the 1950s. They work by forcing your pancreas to pump out more insulin. That drops blood sugar fast-and it’s cheap. Generic glipizide costs less than $5 a month. Compare that to newer drugs like Ozempic, which can run over $500. That’s why, even today, about 15% of U.S. adults with type 2 diabetes still take them, especially those on Medicare or without good insurance. But here’s the catch: these drugs don’t just lower blood sugar. They can make it drop too low-dangerously low. That’s hypoglycemia. And not all sulfonylureas cause it at the same rate.The Big Divide: Long-Acting vs. Short-Acting
Not all sulfonylureas are created equal. The biggest split is between long-acting and short-acting versions. Glyburide (also called glibenclamide) is the most common long-acting one. It sticks around in your body for over 24 hours. Even after you’ve eaten, it keeps pushing insulin out. That’s why so many older adults end up in the hospital with low blood sugar. A 2017 study in Diabetes Care found people on glyburide had nearly three times the risk of severe hypoglycemia compared to those on short-acting versions. Glipizide is the opposite. It works fast and clears out in 4 to 6 hours. It doesn’t linger. That means if you skip a meal or eat less than usual, your blood sugar won’t crash as hard. A 2019 analysis showed glipizide caused only 4.2 episodes of serious hypoglycemia per 1,000 patient-years-less than half the rate of glyburide (12.1 per 1,000). Glimepiride sits in the middle. It lasts longer than glipizide but not as long as glyburide. Still, studies show it carries more risk than glipizide. And gliclazide, not sold in the U.S. but widely used elsewhere, is even more pancreas-specific-meaning it only triggers insulin when blood sugar is high. That’s why it’s often the top pick in Europe and Asia.Who’s at Highest Risk?
If you’re over 65, have kidney trouble, or skip meals often, you’re in the danger zone for sulfonylurea-induced hypoglycemia. The American Geriatrics Society says flat out: don’t prescribe glyburide to anyone 65 or older. Why? Because older kidneys can’t clear the drug well. Glyburide builds up. Its metabolites hang around even longer. One patient story from Reddit tells of a 72-year-old who spent three days in the hospital after his glyburide dose wasn’t lowered when his kidney function dropped. His endocrinologist later admitted: "I never should’ve prescribed that to someone his age." Even if you’re younger, irregular eating habits make things risky. If you work night shifts, travel often, or have a busy schedule where meals are unpredictable, glipizide is the only sulfonylurea worth considering. It’s designed for real life.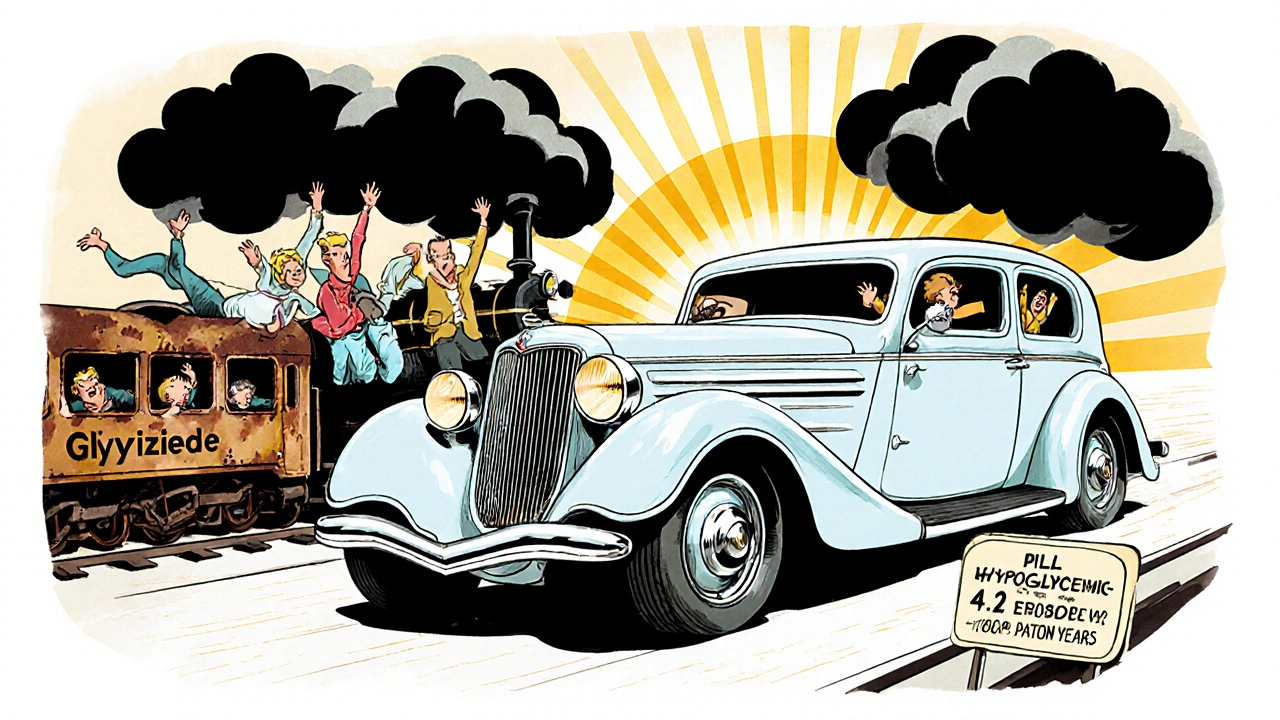
Real People, Real Stories
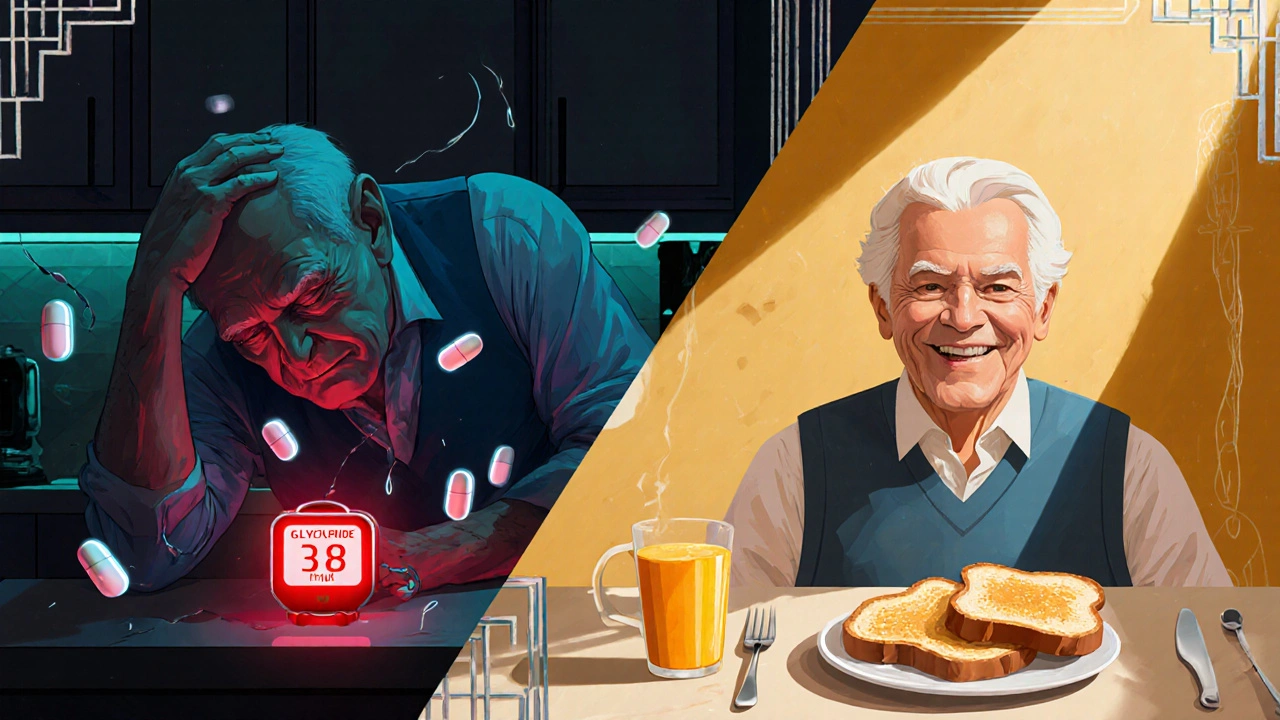
On the American Diabetes Association’s forum, over 80 people shared their switch from glyburide to glipizide. Nearly 75% said they stopped having severe lows. One user wrote: "I was having 2-3 dangerous lows every month on glyburide. Since switching to glipizide, I haven’t had one in six months." Meanwhile, a Reddit thread from 2022 had 68 people talking about glyburide side effects. Over 60% reported ER visits or hospital stays because of low blood sugar. One woman described waking up in the middle of the night with shaking, sweating, and confusion-her blood sugar at 38 mg/dL. She had no idea it was the drug, not her diet. The FDA’s own data backs this up. Between 2018 and 2022, glyburide was responsible for nearly 70% of all sulfonylurea-related hypoglycemia reports-even though it’s only prescribed about one-third of the time. That’s not coincidence. That’s a red flag.What the Experts Say
Dr. Robert Vigersky, a top endocrinologist, put it bluntly: "The question isn’t whether to use sulfonylureas. It’s which one you choose." The American Diabetes Association’s 2024 guidelines now say: "When a sulfonylurea is needed, prefer glipizide over glyburide or glimepiride, especially in older adults or those with unpredictable meals." Dr. Silvio Inzucchi, a Yale professor, says the idea that all sulfonylureas are the same ended in 2016. That’s when a massive UK study proved long-acting ones were nearly three times more likely to cause severe hypoglycemia-with no extra benefit for heart health. But even glipizide isn’t perfect. Dr. John Buse from UNC reminds us: "Compared to newer drugs like SGLT2 inhibitors or GLP-1 agonists, even glipizide carries a high risk of low blood sugar." And he’s right. Newer drugs don’t cause hypoglycemia unless taken with insulin or sulfonylureas. They also help with weight loss and heart protection.How to Use Them Safely
If you’re on a sulfonylurea, here’s what you need to do:- Start low. Glipizide should begin at 2.5 mg-not 5 mg. Glyburide at 1.25 mg-not 5 mg.
- Watch for early signs. Sweating, shaking, hunger, dizziness-these aren’t "just stress." They’re your body screaming for sugar.
- Know the 15-15 rule. If your blood sugar is below 70, eat 15 grams of fast-acting carbs (4 glucose tabs, ½ cup juice, 1 tablespoon honey). Wait 15 minutes. Check again. Repeat if needed.
- Adjust for kidneys. If your eGFR is below 60, avoid glyburide. Glipizide is safer until eGFR drops below 30.
- Never skip meals. Even if you’re not hungry, eat something. A small snack can prevent disaster.
- Alert your doctors. Tell every provider you see-dentist, surgeon, ER staff-that you’re on a sulfonylurea. Hospitalization can trigger dangerous lows.
What’s Changing in 2025?
A new extended-release version of glipizide, Glucotrol XL, just got FDA approval in 2023. It releases the drug slowly, cutting hypoglycemia risk by 32% compared to regular glipizide. That’s huge. The SURE-DM3 trial, tracking 1,200 elderly patients on glipizide vs. gliclazide, will release results in late 2025. Early data suggests gliclazide might be even safer than glipizide. Meanwhile, glyburide use is dropping fast. In 2010, nearly 30% of new diabetes patients got a sulfonylurea. By 2022, that number was under 13%. The shift to safer, more modern drugs is real. But in places where cost is the only barrier-like rural South Africa, parts of India, or low-income communities in the U.S.-sulfonylureas will stick around. That’s why choosing the right one matters more than ever.Bottom Line: What to Do
If you’re on a sulfonylurea:- If it’s glyburide or glimepiride-ask your doctor if you can switch to glipizide.
- If you’re over 65, kidney problems, or have erratic meals-glipizide is your only safe sulfonylurea option.
- If you’re newly diagnosed and cost is an issue-glipizide is still the best sulfonylurea choice.
- If you’re young, healthy, and have stable meals-glipizide is still safer than the alternatives.
- Never assume all sulfonylureas are the same. They’re not.
Diabetes treatment has moved far beyond the 1990s. But for millions, cost still forces a choice. Choosing glipizide over glyburide isn’t just a tweak. It’s the difference between living with low blood sugar-and living without it.
Which sulfonylurea has the lowest risk of hypoglycemia?
Glipizide has the lowest risk of hypoglycemia among commonly used sulfonylureas. Studies show it causes about half the number of severe low blood sugar episodes compared to glyburide. Its short half-life (2-4 hours) means it doesn’t linger in the body, reducing the chance of unexpected lows-especially if meals are skipped. Gliclazide, not available in the U.S., may be even safer but isn’t an option for most patients.
Why is glyburide dangerous for older adults?
Glyburide has a long half-life (up to 10 hours) and produces active metabolites that can last over 24 hours. In older adults, kidney function declines, so the body can’t clear the drug properly. This leads to buildup, causing prolonged insulin release-even when blood sugar is low. The American Geriatrics Society’s Beers Criteria explicitly warns against glyburide in patients over 65 due to this risk. Studies show glyburide causes nearly 20 serious hypoglycemia episodes per 1,000 patient-years in seniors-versus under 4 for glipizide.
Can I switch from glyburide to glipizide safely?
Yes, switching from glyburide to glipizide is not only safe-it’s often recommended. Start with glipizide 2.5 mg once daily, usually before breakfast. Your doctor may reduce your glyburide dose gradually or stop it immediately, depending on your blood sugar control. Most patients report fewer low blood sugar episodes within weeks. Monitor your levels closely for the first two weeks after switching.
Are there alternatives to sulfonylureas with less hypoglycemia risk?
Yes. SGLT2 inhibitors (like empagliflozin) and DPP-4 inhibitors (like sitagliptin) have much lower hypoglycemia risk because they don’t force insulin release. GLP-1 receptor agonists (like semaglutide) rarely cause lows unless combined with insulin or sulfonylureas. These newer drugs also offer heart and kidney benefits. But they cost 10-100 times more than glipizide. If cost is a barrier, glipizide remains the safest sulfonylurea option.
What should I do if I experience low blood sugar on a sulfonylurea?
If you feel shaky, sweaty, dizzy, or confused, check your blood sugar immediately. If it’s below 70 mg/dL, consume 15 grams of fast-acting carbs: 4 glucose tablets, ½ cup juice, or 1 tablespoon of honey. Wait 15 minutes, then check again. If still low, repeat. Once stable, eat a snack with protein and carbs (like peanut butter on toast). Tell your doctor about the episode-it may mean your dose needs adjusting. Never ignore repeated lows.
Is glipizide safe for people with kidney disease?
Glipizide is one of the safest sulfonylureas for kidney disease. It doesn’t rely on kidney clearance for elimination. No dose adjustment is needed until eGFR drops below 30 mL/min/1.73m². Glyburide and glimepiride, however, should be avoided once eGFR falls below 60. Always have your kidney function checked before starting or changing sulfonylureas.
Why do some doctors still prescribe glyburide?
Some doctors still prescribe glyburide out of habit, lack of awareness, or because it’s cheaper. But evidence shows it’s riskier. A 2024 audit found nearly 30% of Medicare patients over 80 were still on glyburide-despite clear guidelines against it. Insurance formularies sometimes favor glyburide because it’s the cheapest generic. But cost savings are meaningless if the patient ends up in the hospital. More doctors are switching to glipizide as awareness grows.
Man, I wish my doc had told me this 3 years ago. I was on glyburide and had three ER trips in 18 months. Thought I was just bad at eating on time. Turns out my meds were trying to kill me slowly. Switched to glipizide and haven’t had a single scare since. Seriously, if you’re on glyburide and still breathing - get off it.
Oh wow, so now we’re villainizing glyburide because it’s old? Next you’ll tell me penicillin’s dangerous because it doesn’t cure cancer. People have survived on this stuff for 70 years. Maybe your body’s just weak. Or maybe you’re one of those people who thinks every drug should come with a 30-page warning label and a therapist.
Statistically speaking, the 2017 Diabetes Care study cited has a 95% CI of 2.1–4.3 for severe hypoglycemia risk differential - yet the author conflates relative risk with absolute risk. The NNT to prevent one severe episode by switching from glyburide to glipizide is approximately 83. That’s not life-changing - it’s statistically marginal. And let’s not ignore confounding variables: adherence, diet variability, and renal function trajectories. This is fearmongering dressed as clinical guidance.
Look, if you’re from India or South Africa and you can’t afford Ozempic, you’re not getting some fancy new drug. You’re getting what works - and glyburide works. Americans act like they’re entitled to the safest, most expensive option. Meanwhile, the rest of the world is living with this and still managing. Stop acting like every old drug is a death sentence. We didn’t need all this ‘evidence’ 30 years ago - and we don’t need it now.
glipizide = life saver 😭 I was having night sweats, shaking, crying in the dark thinking I was dying… switched and now I sleep like a baby 🙏 no more 3am panic attacks. my endo was like ‘yeah you should’ve switched sooner’… dumbass. 💔
im not saying glyburide is bad but like… why do ppl always act like glipizide is magic? its still a sulfonylurea. still makes ur pancreas work. still can cause lows. if u r that scared of hypoglycemia why not just go metformin and walk more? jfc.
I’ve been on glipizide for 5 years now. Started at 2.5mg like they said. Had a few lows at first, but learned the 15-15 rule. My A1c dropped from 8.2 to 6.8. My kidney numbers are stable. I’m 71. No ER visits. No hospital stays. This isn’t rocket science - just common sense. Docs need to stop being lazy and start listening to the data. And yes, I spelled everything right.
Let’s be clear: this is a classic case of guideline creep disguised as medical progress. The FDA didn’t ban glyburide. The ADA didn’t ban it. Yet somehow, we’re now treating it like thalidomide. Meanwhile, the real issue - poor patient education, inconsistent meal timing, and lack of glucose monitoring - is being ignored. It’s easier to blame the drug than to fix the system. And don’t even get me started on the pharmaceutical industry’s quiet push to replace generics with branded biologics…
There’s something deeply human about this whole conversation. We’re not just talking about pharmacokinetics - we’re talking about dignity. The elderly patient who forgets to eat because they’re lonely. The single mom working two jobs who skips lunch because she can’t afford the time. The immigrant who can’t afford insulin but can afford a $5 pill. Glipizide isn’t just safer - it’s kinder. It gives people back control without demanding perfection. That’s not medicine. That’s mercy.
As a clinical pharmacist, I’ve seen this play out too many times. Glyburide is a relic with a death sentence attached - especially in renal impairment. Glipizide’s hepatic metabolism makes it the only viable sulfonylurea in CKD stages 3-4. And yes, the new extended-release version? Game-changer. 32% reduction in hypoglycemia? That’s not noise - that’s a clinical win. But here’s what no one’s saying: if we’re going to keep prescribing sulfonylureas at all, we need mandatory patient education modules. No more handing out scripts like candy. This isn’t 1998 anymore.