Bone Health Risk Calculator
Your Bone Health Risk Assessment
When we talk about Smoking is the inhalation of tobacco smoke containing nicotine, tar, carbon monoxide, and thousands of other chemicals, we often focus on lungs and heart. Yet bone health suffers quietly in the background. Bone is a living tissue that constantly remodels, providing structure, protecting organs, and storing minerals like calcium. This article breaks down the ways smoking attacks bone, the real‑world impact on osteoporosis and fractures, and what you can do to safeguard your skeleton.
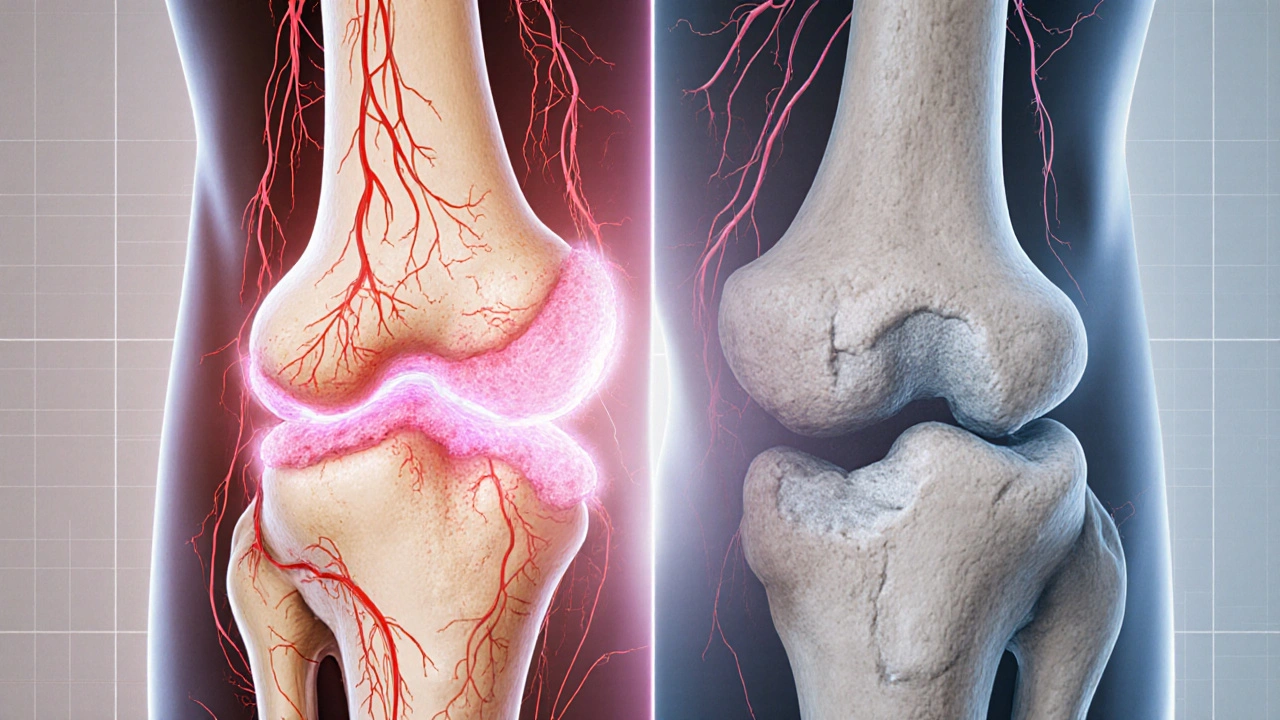
Why Smoke Undermines Bone Structure
Three biological tricks make smoking a bone‑killer:
- Vasoconstriction: Carbon monoxide binds hemoglobin, reducing oxygen delivery to bone‑forming cells (osteoblasts). Less oxygen means slower matrix production.
- Hormone disruption: Nicotine (Nicotine is a potent stimulant that alters estrogen, testosterone, and cortisol levels) lowers estrogen in women and interferes with calcium metabolism, both essential for bone density.
- Inflammatory overload: Smoke introduces free radicals that trigger chronic inflammation, speeding up bone resorption (breakdown) by osteoclasts.
These mechanisms combine to tip the remodeling balance toward loss, leaving the skeleton frail over time.
Impact on Bone Mineral Density and Osteoporosis
Bone mineral density (BMD) measures the amount of mineral packed into a given area of bone. Studies across continents consistently show that long‑term smokers have BMD scores 5‑12% lower than never‑smokers of the same age and sex. The gap widens after age 50, when natural bone loss accelerates.
Lower BMD translates directly into higher Osteoporosis is a condition where bones become porous and fragile, increasing fracture risk rates. In a 2023 meta‑analysis of 27 cohort studies, smokers were 1.5 times more likely to develop osteoporosis than non‑smokers, even after adjusting for diet and activity.
Smoking Slows Fracture Healing
If a smoker does break a bone, the story doesn’t end at the break. Healing time can stretch from the typical 6‑8 weeks to 12‑16 weeks or longer. The same vasoconstriction that starves osteoblasts also impairs blood clot formation, a crucial first step in repair. Nicotine’s interference with collagen synthesis delays the formation of the soft callus that bridges the fracture.
Clinicians often report higher rates of non‑union (failure to heal) in smokers. One orthopedic center tracked 1,200 tibial fractures and found a 30% non‑union rate among smokers versus 10% in non‑smokers.
Oral Bone Health: Periodontal Disease Connection
Smoking also harms the jawbone through Periodontal disease is a chronic gum infection that destroys the bone supporting teeth. The reduced blood flow and immune suppression make the gums a perfect breeding ground for bacteria. Over years, the alveolar bone recedes, leading to tooth loss and a visible sign that the skeleton is under attack.
Nutrition, Lifestyle, and the Smoking Effect
Good nutrition can blunt some smoke‑related damage, but it can’t fully offset it.
- Calcium is the primary mineral stored in bone, essential for strength and remodeling intake above 1,200mg/day is recommended for smokers over 40.
- Vitamin D is a fat‑soluble vitamin that enhances calcium absorption and supports bone formation levels should stay above 30ng/mL; many smokers need supplementation.
- Weight‑bearing exercise (e.g., brisk walking, resistance training) stimulates osteoblast activity, partially counteracting nicotine’s suppression.
Even with optimal diet and exercise, the bone‑damage signal from smoking remains significant, underscoring the need for cessation.
Benefits of Quitting: Bone Recovery Timeline
The good news: bone health starts to bounce back soon after the last cigarette.
- Within 3 months: Blood flow improves, delivering more oxygen and nutrients to bone cells.
- 6-12 months: BMD gains of 1‑2% have been documented, especially in women who combine quitting with calcium/vitamin D supplementation.
- 2-5 years: Fracture risk approaches that of never‑smokers, though former heavy smokers may retain a modest residual risk.
These gains are amplified when quitting is paired with a bone‑friendly lifestyle.

Practical Steps to Protect Your Bones
If you’re not ready to quit, here are actions that can limit damage:
- Limit cigarette count: Even cutting down reduces carbon monoxide exposure and improves oxygen delivery.
- Boost calcium & vitamin D: Aim for dairy, leafy greens, fortified foods, and consider a 1,000IU vitamin D supplement daily.
- Stay active: 30 minutes of weight‑bearing activity most days keeps osteoblasts busy.
- Dental hygiene: Brush twice daily, floss, and see a dentist regularly to catch early periodontal changes.
- Regular BMD screening: If you’re over 40 and a smoker, ask your doctor for a DEXA scan every 2‑3 years.
Ultimately, Smoking cessation is the most powerful intervention to halt bone loss and reduce fracture risk. Programs that combine counseling, nicotine replacement, and lifestyle coaching have quit rates up to 35% at 12 months.
Key Takeaways
- Smoking cuts oxygen, disrupts hormones, and fuels inflammation, all of which erode bone.
- Smokers lose 5‑12% more bone density and face a 50% higher osteoporosis risk.
- Fracture healing is significantly slower, and oral bone loss leads to periodontal disease.
- Calcium, vitamin D, and weight‑bearing exercise can mitigate but not eliminate damage.
- Quitting reverses many effects; bone density can improve within a year.
Comparison: Bone Health in Smokers vs. Non‑Smokers
| Metric | Smokers | Non‑Smokers |
|---|---|---|
| Bone Mineral Density (g/cm²) | −5% to −12% lower | Baseline |
| Osteoporosis prevalence | 1.5× higher | Reference |
| Fracture healing time | 12‑16 weeks | 6‑8 weeks |
| Annual fracture risk | 30% increase | Baseline |
| Periodontal bone loss (mm/year) | 0.8mm | 0.2mm |
Frequently Asked Questions
How quickly does smoking affect bone density?
Bone density begins to decline within a few years of daily smoking. A longitudinal study showed measurable BMD loss after just 5 years of habit.
Can nicotine patches still harm my bones?
Nicotine alone can affect hormone balance, but the dose in patches is much lower than cigarettes. Most research suggests patches pose minimal bone risk, especially when paired with calcium and vitamin D.
Do e‑cigarettes damage bone the same way?
E‑cigarettes deliver nicotine without tar, but they still cause vasoconstriction and oxidative stress, which can impair bone health. Long‑term data are limited, so caution is advised.
Is bone loss reversible after I quit?
Yes. Within the first year of cessation, many former smokers regain 1‑2% BMD, and fracture risk drops toward that of never‑smokers after 2‑5 years.
Should I get a DEXA scan if I smoke?
If you’re over 40 or have other risk factors (family history, low calcium intake), a DEXA scan every 2‑3 years is advisable to monitor bone density.
How does smoking affect the jawbone?
Smoking accelerates periodontal disease, leading to alveolar bone loss. This can cause loose teeth and complicate dental implants.

Thanks for pulling together all that info! It's eye‑opening how smoking sneaks into bone health, not just lungs. I love how you broke down the hormone and inflammation bits – makes it real easy to understand. If anyone's looking to cut back, swapping a pack for a walk can already boost oxygen to bone cells.
The article dramatically overstates the impact of smoking on skeletal health.
Look, this whole bone thing is just a ploy by big pharma to scare us. Smoking ain't the only poison out there, yet they love to blame it. Anyway, keep your calcium high, that's the real fix.
Interesting breakdown; the vasoconstriction part really caught my eye. I’ve noticed my own recovery slows when I’m stuck behind a smoker at the gym. The link between nicotine and estrogen is something I didn't know existed. It’s surprising how quickly bone density can shift with lifestyle changes. Maybe we should push for more public awareness about this.
The data presented are indeed compelling; however, one must consider confounding variables, such as dietary calcium intake, physical activity levels, and genetic predisposition. Moreover, the statistical significance of the cited studies should be scrutinized before drawing definitive conclusions.
The connection between smoking and periodontal disease is often missed. It’s a clear sign that the oral cavity mirrors systemic bone loss. Regular dental check‑ups can catch this early.
Even a few cigarettes a day sabotage bone remodeling. Quitting is the only real solution.
Smoking hurts your bones. Stop it.
What they don't tell you is that the tobacco industry funds many of these studies to keep us buying. The real agenda is to keep us dependent. Look beyond the headlines.
Smoking's impact on bone health is often overlooked, yet the evidence is overwhelming.
Chronic exposure to nicotine and carbon monoxide reduces oxygen supply to osteoblasts, slowing new bone formation.
Hormonal disruptions, particularly lowered estrogen, further diminish bone density, especially in women.
Inflammatory pathways activated by tobacco smoke accelerate osteoclast activity, leading to heightened bone resorption.
Epidemiological studies across continents have consistently shown a 5‑12% reduction in BMD among smokers.
This reduction translates into a markedly higher risk of osteoporosis, with smokers being roughly 1.5 times more likely to develop the condition.
Moreover, fracture healing times are significantly prolonged, often doubling the typical recovery period.
The impaired vascularization caused by smoking also hampers the initial clot formation essential for bone repair.
Calcium and vitamin D supplementation can mitigate some damage but cannot fully counteract the detrimental effects of nicotine.
Weight‑bearing exercise remains a valuable countermeasure, stimulating osteoblast activity despite nicotine's presence.
Nevertheless, the most effective intervention remains smoking cessation, which begins to restore vascular function within three months.
Bone mineral density improvements of 1‑2% are observable within six to twelve months after quitting, especially when coupled with adequate nutrition.
Long‑term abstinence further narrows the fracture risk gap, approaching that of never‑smokers after five years.
For individuals over forty, regular DEXA scans are advisable to monitor bone health trajectory.
Dental health is also a barometer; periodontal disease can signal accelerated alveolar bone loss in smokers.
Ultimately, the synergy of quitting, proper diet, and exercise offers the best prognosis for skeletal integrity.
Your bones feel the pain, just like my heart.
If you think smoking is just a habit, think again; it's a moral failing affecting future generations. People who care about their kids should quit today. Health isn't a personal choice, it's a social responsibility.
The science is clear, yet some still deny it. Bone loss is real.
The physiological mechanisms are intricate, yet comprehensible when examined closely. Osteoblasts require adequate oxygen, which smoking deprives them. Hormonal imbalances further exacerbate mineral loss. Addressing these factors holistically yields the best outcomes.
Believe it or not, even a typo‑laden positive outlook can help you stick to a quit plan. Celebrate each smoke‑free day, however small. Persistence beats perfection.
The bone whispers in silence; we ignore its cries while lighting up. In the drama of life, the skeleton is the unsung hero, bearing the weight of every habit. When smoke clouds our veins, it also clouds the very foundation that holds us. Wake up, the bones are screaming.
Great summary, thanks!
While the article is thorough, it lacks a practical step‑by‑step guide for quitting. Readers need actionable plans, not just statistics. Also, the tone borders on preachy, which may alienate smokers seeking help. A balanced approach would be more effective.