Colesevelam Side Effect Risk Calculator
This tool estimates your risk of experiencing constipation while taking colesevelam based on key risk factors. The FDA and Mayo Clinic identify these factors as important indicators of potential issues.
When you're taking colesevelam for diabetes or high cholesterol, the last thing you want is to spend your days feeling bloated or stuck. It’s a common problem-about 1 in 10 people on this medication report constipation, and nearly as many deal with bloating or gas. What makes it confusing is that colesevelam is also used to treat diarrhea in some patients. How can one drug fix loose stools for some and cause hard ones for others? The answer lies in how your body handles bile acids-and whether you already have a slow digestive system.
Why Colesevelam Causes Constipation
Colesevelam works by binding bile acids in your gut. These acids help digest fat, and when they’re pulled out of circulation, your liver pulls more cholesterol from your blood to make new ones. That’s good for lowering cholesterol and helping control blood sugar in type 2 diabetes. But here’s the catch: bile acids also help keep stools soft. When too many are removed, your stool becomes dry and hard. That’s constipation. Unlike older bile acid sequestrants like cholestyramine, colesevelam is designed to be gentler. It doesn’t form gritty clumps in your gut like the older drugs did. Instead, it turns into a soft gel. But even this improved version still removes enough bile acid to slow things down. In clinical trials, 10-15% of people taking colesevelam had constipation severe enough to notice. For some, it’s mild. For others, it’s a daily struggle.Bloating and Gas: The Other Common Issue
Bloating and flatulence happen because your gut bacteria start fermenting undigested material. When bile acids are bound by colesevelam, fats aren’t broken down as well. That means more fat reaches the colon, where bacteria feast on it-and produce gas. You might feel full, swollen, or even painful after meals, even if you haven’t eaten much. This isn’t just discomfort-it can make you avoid meals or feel embarrassed. Many patients report bloating within the first week of starting the drug. The good news? It often gets better over time. Your gut adjusts. But if it doesn’t, you need to act.Who’s Most at Risk?
Not everyone gets these side effects. Some people take colesevelam for years with no issues. Others develop problems quickly. The biggest risk factor? Pre-existing constipation. If you’ve ever had slow transit constipation, irritable bowel syndrome with constipation (IBS-C), or a history of fecal impaction, colesevelam can make things much worse. The FDA and Mayo Clinic both warn against using it in people with bowel blockages or motility disorders. A 2024 study in Alimentary Pharmacology & Therapeutics found that people with Bristol Stool Scale scores of 3 or lower (meaning hard, lumpy stools) were more than three times as likely to develop serious constipation on colesevelam. Another red flag: opioid use. If you’re taking pain meds that slow your gut, adding colesevelam is like pouring gasoline on a fire. The European Medicines Agency now specifically flags opioid-induced constipation as a concern.How to Manage Constipation Without Stopping the Drug
You don’t have to quit colesevelam if you’re having trouble. Many people stay on it successfully with simple adjustments. Start low, go slow. The Royal Marsden NHS protocol recommends beginning with just 1.25 grams per day (two 625 mg tablets) with your largest meal. After seven days, increase to 2.5 grams. After another week, go to the full 3.75 grams. This gives your gut time to adapt. Jumping straight to the full dose increases your risk of constipation by nearly 40%. Drink more water. Colesevelam absorbs water in your gut. If you’re not drinking enough, your stool will dry out faster. Aim for at least 8 cups (2 liters) of water daily. Add a glass with every dose. Add soluble fiber. Psyllium (Metamucil) is the top choice. It doesn’t get broken down by bacteria, so it doesn’t cause extra gas. It also holds water and softens stool. One patient on an IBS forum shared that after starting colesevelam, their 10+ daily watery stools stopped-but they needed 17 grams of psyllium daily to avoid becoming constipated. That’s about 3 teaspoons of psyllium powder, taken with plenty of water. Use stool softeners if needed. Docusate sodium (Colace) is safe to use with colesevelam. It helps water stay in your stool. Avoid stimulant laxatives like senna or bisacodyl-they can cause cramping and electrolyte imbalances, especially if you’re also on diabetes meds. Take it with meals. While colesevelam should be taken 4 hours before or after other medications (to avoid binding them), taking it with food can help reduce bloating. The food slows its movement through the gut, reducing sudden bile acid binding that triggers gas.What to Avoid
Don’t try to tough it out. If you haven’t had a bowel movement in 3 days, contact your doctor. Fecal impaction is rare but serious. One WebMD review described an ER visit for impaction after just 5 days on colesevelam-because their doctor didn’t ask about their history of slow digestion. Also, don’t assume fiber supplements will fix everything. Insoluble fiber like wheat bran can make bloating worse. Stick to soluble fiber: psyllium, oats, flaxseed, and chia. And avoid large amounts of dairy or fatty foods-they can increase gas production when bile acids are low.When to Consider Switching
If you’ve tried all the above and still can’t tolerate the side effects, talk to your doctor about alternatives. Cholestyramine is cheaper-about $50 a month-but causes constipation in up to 39% of users. It’s grittier, harder to swallow, and more likely to cause nausea. Colesevelam is still the better-tolerated option overall. Newer drugs like elobixibat (not available in the U.S.) target bile acid reabsorption differently and may have fewer GI side effects. Rifaximin is sometimes used off-label for bile acid diarrhea, but it’s not approved for diabetes. For now, colesevelam remains the first-line choice for bile acid diarrhea and cholesterol control because it’s the most tolerable. About 65% of new prescriptions in the U.S. go to colesevelam-not because it’s perfect, but because the alternatives are worse.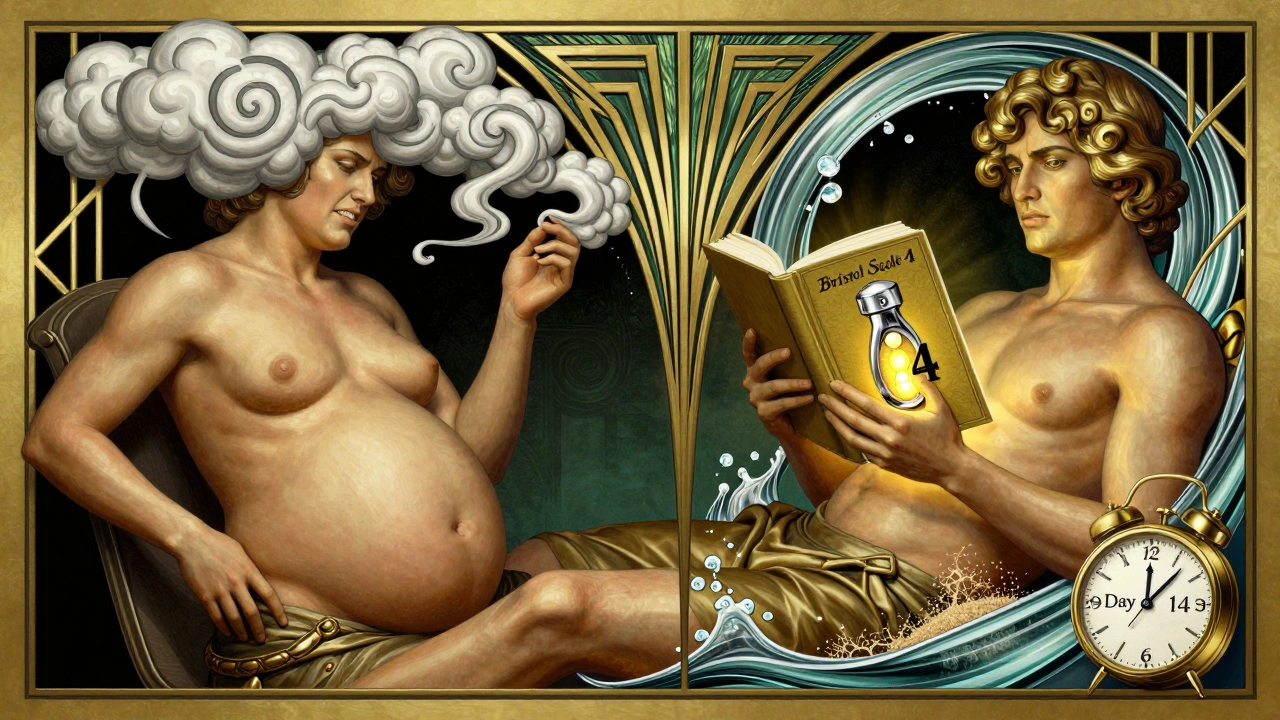
Monitoring and Long-Term Use
If you’re on colesevelam long-term, ask your doctor about checking your stool pattern. Keep a simple log: number of bowel movements per day, consistency (use the Bristol Stool Scale), and any bloating or pain. This helps spot problems early. Blood tests for serum C4 (a marker of bile acid production) are becoming more common. Patients with low C4 levels (<15 ng/mL) are at higher risk for constipation. If your doctor offers this test, it can help predict whether you’ll need a lower dose. Sanofi is working on a new delayed-release version of colesevelam that releases the drug farther down the gut, where it’s less likely to cause constipation. Phase I trials start in early 2025. Until then, smart management is your best tool.Real Stories, Real Solutions
One patient in Durban, South Africa, started colesevelam for diabetes and high cholesterol. Within days, she went from regular bowel movements to going every 4-5 days. She tried prune juice-no help. Then she added 10 grams of psyllium daily, drank more water, and moved to a lower dose (2.5g instead of 3.75g). Within two weeks, she was back to daily, soft stools. She’s been on it for 18 months now, with no issues. Another man, 68, had a history of slow transit constipation. His doctor didn’t ask about it. He started colesevelam and ended up in the ER with impaction. His story isn’t rare. That’s why doctors now screen for constipation history before prescribing.Bottom Line
Colesevelam can cause constipation and bloating-but it doesn’t have to stop you from taking it. Most side effects are manageable with the right steps: start low, drink water, use soluble fiber, and listen to your body. If you’ve had constipation before, tell your doctor. Don’t assume it’ll be fine. With the right approach, you can keep the benefits of colesevelam without the discomfort.Can colesevelam cause severe constipation?
Yes, colesevelam can cause severe constipation, especially in people with a history of slow bowel movements or existing constipation. About 10-15% of users report constipation in clinical trials, and in rare cases, it can lead to fecal impaction requiring emergency care. Always tell your doctor if you’ve had constipation before starting this medication.
How long does it take for colesevelam side effects to go away?
Bloating and gas often improve within 2-4 weeks as your gut adjusts. Constipation may take longer, especially if you’re on the full dose. Gradual dose escalation over 14 days helps reduce this risk. If constipation doesn’t improve after a month, talk to your doctor about lowering the dose or adding fiber.
Is it safe to take laxatives with colesevelam?
Stool softeners like docusate sodium are safe to use with colesevelam. Avoid stimulant laxatives like senna or bisacodyl-they can cause cramps and electrolyte imbalances. Always take colesevelam at least 4 hours before or after other medications, including laxatives, to avoid interactions.
Can colesevelam help with diarrhea too?
Yes, colesevelam is used to treat bile acid diarrhea, a condition common after gallbladder removal, Crohn’s disease, or radiation therapy. It binds excess bile acids that cause watery stools. The same mechanism that helps diarrhea can cause constipation in people without bile acid malabsorption. That’s why it’s not used for everyone with digestive issues.
What’s the best fiber to take with colesevelam?
Soluble fiber is best-especially psyllium husk (Metamucil). It softens stool without increasing gas. Avoid insoluble fiber like wheat bran, which can worsen bloating. Start with 5-10 grams daily, mixed in water or juice. Take it at least 2 hours apart from colesevelam to avoid binding.
Should I stop colesevelam if I get constipated?
Not necessarily. Many people continue taking it with lifestyle changes like more water, fiber, and a lower dose. Only stop if you haven’t had a bowel movement in 3 days, have severe pain, or notice blood in your stool. Always consult your doctor before stopping any medication.

colesevelam is just a fancy name for a bile acid sponge, bro. it doesnt digest fat so your gut bacteria throw a rave on the undigested grease and boom - gas city. i started at 3.75g day one and regretted it. now i do 1.25g with dinner and drink a whole liter of water. no more rock-hard poop. psyllium is your new best friend, not some magic fiber fairy.
you people are so naive. this drug was designed by pharma to keep you dependent. they know constipation makes you go back for more meds - laxatives, stool softeners, colon cleanses. it’s a cycle. the real fix? stop taking it. your liver doesn’t need to make bile from cholesterol. your body’s fine. you’re just addicted to the illusion of control.
did you know the FDA approved this without long-term gut motility studies? and yet they tell us it’s safe for diabetics? what about the 2023 whistleblower report from the FDA’s GI division? they flagged colesevelam as a potential contributor to colonic inertia in elderly patients - but it got buried under ‘risk-benefit analysis.’ i’ve seen three patients with impaction. none were warned. this isn’t medicine. it’s corporate negligence wrapped in a white coat.
why are we even talking about this? just switch to ezetimibe. cheaper, no constipation, same cholesterol drop. why do doctors keep prescribing this gritty mess? laziness. they don’t wanna look up alternatives. it’s not rocket science.
in india we use cholestyramine more often and its worse but cheaper. people here just drink more water and eat papaya. no psyllium needed. why do americans always need a supplement for everything? your gut is not broken. you just eat too much processed food and then wonder why the drug makes it worse.
look i’ve been on this for 4 years… 1.25g in morning with oatmeal and 2.5g at night with dinner… i drink 3 liters of water daily… i take psyllium husk 10g at night… i dont take dairy… i avoid fried stuff… i still get bloated after 7pm… but i dont care… my LDL is 85… my HbA1c is 5.8… i’ll take bloating over a heart attack any day… you people don’t get it… this isn’t about comfort… it’s about survival
i took this for 3 weeks and gave up. constipation was awful. tried everything. even drank prune juice. nothing. just stopped it. my cholesterol went up a bit but honestly? i feel better. why do we think we have to suffer for a number?
if you can’t handle a little constipation you shouldn’t be on meds. life isn’t supposed to be easy. get stronger. your gut will adapt. stop whining. and stop blaming the drug. blame your poor diet. you eat too much sugar. that’s why your digestion is trash.
psyllium + water = magic 🌱💧 i started at 5g, now i do 12g. no bloating, no gas, just smooth. colesevelam is a beast but you can tame it. also, try magnesium citrate 200mg at night. not a laxative, just a gentle helper. my gut loves it. 🙏
the key here is bile acid dynamics - it’s not just about quantity but timing and individual bile acid pool size. patients with low C4 levels or elevated 7α-hydroxy-4-cholesten-3-one are at higher risk for constipation because their bile acid synthesis is already suppressed. adding a sequestrant pushes them into negative balance. that’s why the Bristol Stool Scale is so critical - it’s a direct proxy for bile acid availability. psyllium works because it’s a hydrophilic colloid that doesn’t ferment, unlike inulin or FODMAPs. it’s not about fiber quantity - it’s about fiber quality and bile acid homeostasis. if you’re on this long-term, monitor C4 and consider a bile acid binding capacity test. most docs don’t know this - but you should.
in the grand ontological scheme of human physiology, the ingestion of synthetic bile acid sequestrants represents a profound disruption of the enterohepatic circulation - a delicate feedback loop that has evolved over millennia to maintain lipid homeostasis. when we interfere with this system through pharmacological intervention, we are not merely treating cholesterol - we are altering the very rhythm of digestion, forcing the colon into a state of dysbiosis and stasis. the constipation is not a side effect - it is the inevitable consequence of our hubris in believing we can manipulate nature without cost. perhaps the real question is not how to manage the constipation - but whether we should be taking this drug at all.
americans are weak. drink water. eat fiber. move your butt. problem solved. this drug is fine. if you can’t handle it, go back to eating donuts. we don’t need coddling. fix yourself.
if you’re from india and on this med - skip the psyllium and just eat soaked fenugreek seeds in the morning. 1 tsp soaked overnight, chew it. it’s natural, cheap, and works better than any supplement. also drink warm water with lemon. gut resets in 3 days. no need for fancy western pills. our grandmas knew this before pharma did
i’ve been a nurse for 18 years. i’ve seen patients on colesevelam for over a decade. the ones who do well? they’re the ones who track their stools. they know their Bristol score. they drink water like it’s oxygen. they don’t wait until they’re blocked to act. if you’re on this, treat it like a marathon - not a sprint. start low, stay hydrated, listen to your body. and if you’re on opioids? talk to your doctor. don’t just assume it’s normal. it’s not. your gut is screaming. listen.