Every year, thousands of people end up in emergency rooms because they took what they thought was a harmless pain reliever. It’s not a drug they bought illegally. It’s not some mysterious chemical. It’s something most of us keep in our medicine cabinets: acetaminophen. You’ve probably seen it on the label of Tylenol, NyQuil, Excedrin, or even your cold medicine. But here’s the truth: if you don’t know how much you’re taking, or if you’re mixing it with other meds or alcohol, you’re putting your liver at serious risk.
Why Acetaminophen Is More Dangerous Than You Think
Acetaminophen - also called paracetamol - is one of the most common pain relievers in the world. It’s in over 600 different medications, from fever reducers to sleep aids. That’s the problem. Most people think, “I only took one pill,” and don’t realize they’ve already hit their limit because they took it in three different products that day.
The liver breaks down acetaminophen, turning it into harmless waste. But when you take too much - more than 4,000 mg in a day - the liver gets overwhelmed. It starts producing a toxic byproduct called NAPQI. Normally, your liver uses an antioxidant called glutathione to neutralize it. But if you’ve taken too much acetaminophen, or if you drink alcohol regularly, your glutathione runs out. Then NAPQI starts destroying liver cells. This isn’t slow damage. It can happen in hours.
In the U.S., acetaminophen causes about 56,000 emergency room visits, 26,000 hospital stays, and nearly 500 deaths every year. And here’s the scary part: nearly half of those cases aren’t from people trying to overdose. They’re from people who just didn’t know they were taking too much.
What’s a Safe Dose? It Depends on You
If you’re healthy, the official daily limit is 4,000 mg. That’s eight extra-strength pills (500 mg each) or 12 regular-strength tablets (325 mg each). But that number isn’t the same for everyone.
- People with liver disease - even mild fatty liver - should stay under 2,000 mg per day. Some experts say 1,500 mg is safer.
- People who drink alcohol - even just one drink a day - should also cap intake at 2,000 mg. Alcohol and acetaminophen team up to make liver damage much more likely.
- People taking other medications - especially those for epilepsy, TB, or seizures - may process acetaminophen faster, but that doesn’t mean they can take more. It just means their liver is under more stress.
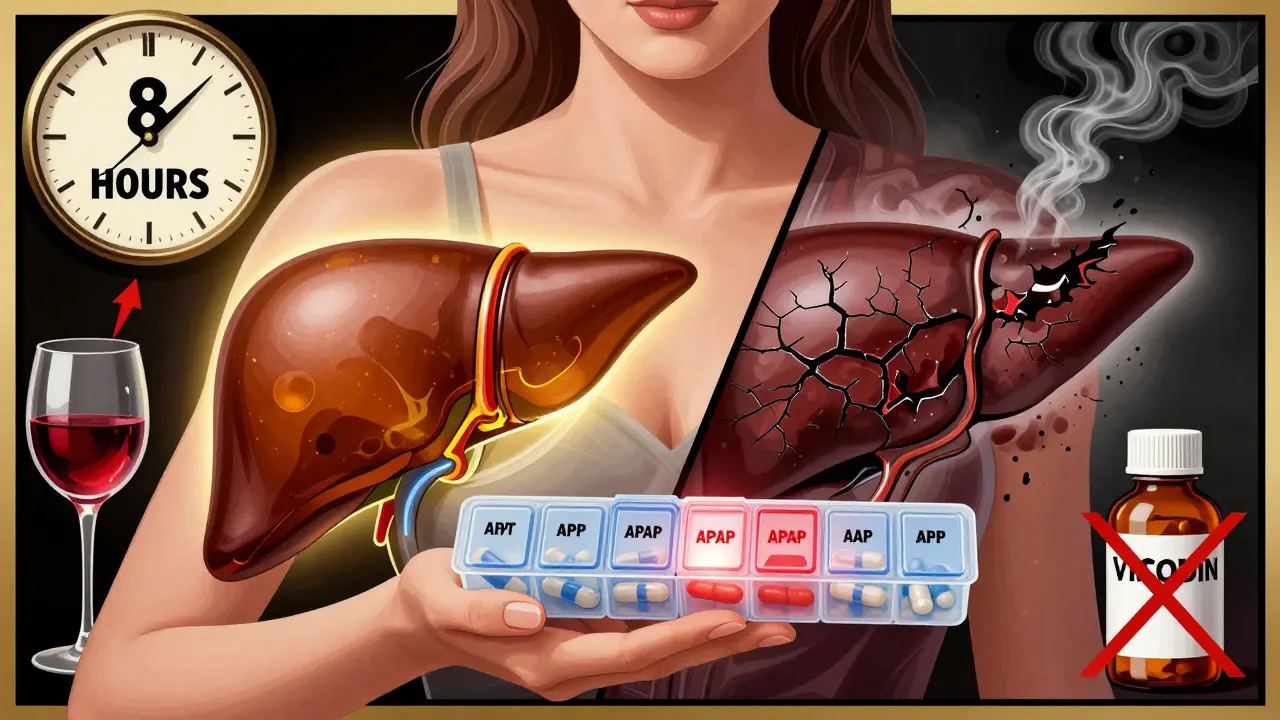
And here’s something most people miss: prescription painkillers like Vicodin or Percocet also contain acetaminophen. So if you’re taking those on top of Tylenol, you’re doubling up without realizing it.
NSAIDs Aren’t the Safe Alternative You Think
Many people switch to ibuprofen or naproxen thinking they’re safer for the liver. They’re not. NSAIDs like Advil, Aleve, and diclofenac don’t usually hurt the liver directly - but they can cause serious problems elsewhere. They raise your risk of stomach bleeding, kidney damage, and high blood pressure. And if you already have liver disease, NSAIDs can make kidney problems worse, which then puts even more strain on your liver.
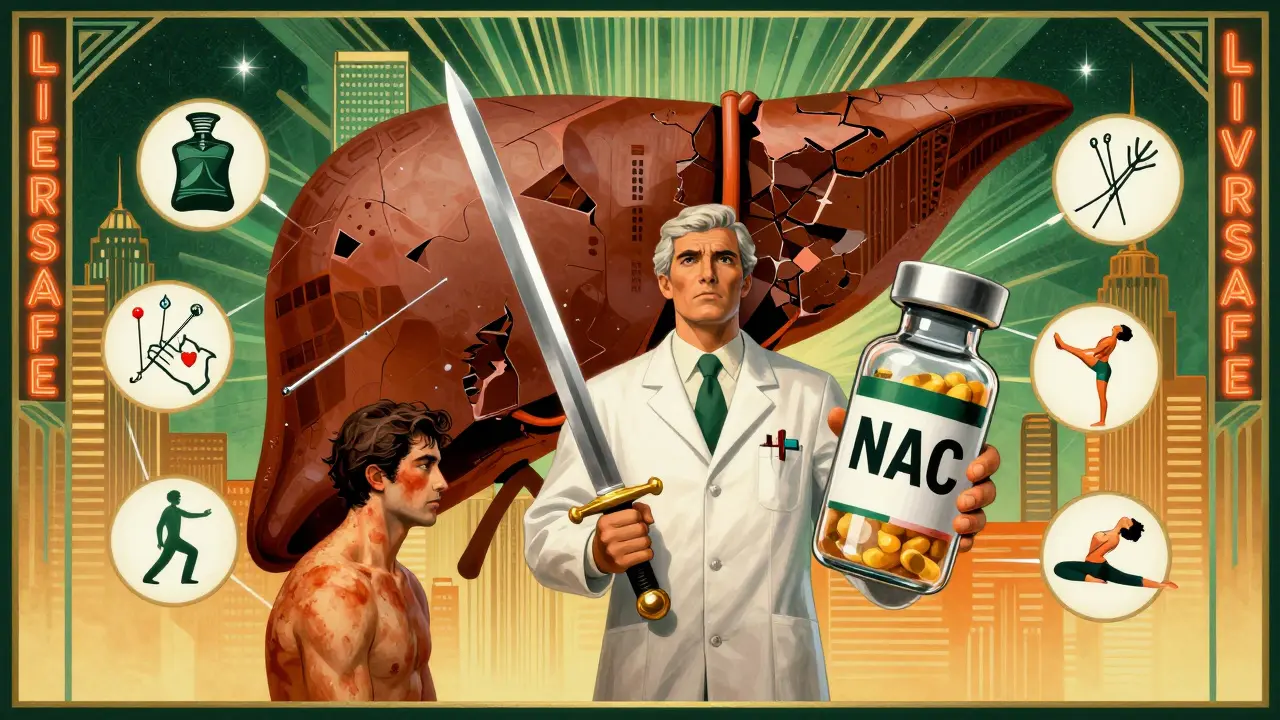
So what’s the answer? Don’t just swap one drug for another. Think about alternatives. For joint pain, try a topical NSAID gel. It doesn’t go through your liver at all. For headaches or mild pain, consider non-drug options like heat packs, gentle stretching, or even acupuncture. The American Liver Foundation now recommends these as first-line treatments for chronic pain.
How to Avoid Accidental Overdose
Most overdoses happen because people don’t read labels. Here’s how to stay safe:
- Check every pill bottle - including cold, flu, and sleep meds. If it says “acetaminophen,” “APAP,” or “paracetamol,” it’s the same thing.
- Never take more than one product with acetaminophen at once. That includes prescription and OTC.
- Use a pill organizer with daily limits. Put only what you’re allowed to take in one day. No more.
- Avoid alcohol completely while using acetaminophen. Even one glass of wine can drop your safe limit from 4,000 mg to 2,000 mg.
- Wait at least 8 hours between doses. Taking it every 4 hours might feel like you’re staying ahead of the pain, but it’s how people accidentally overdose.
Also, don’t assume “natural” or “herbal” pain relievers are safer. Some supplements like kava, green tea extract, or high-dose vitamin A can also damage the liver. Always talk to your doctor before trying new supplements.
Know the Warning Signs
Liver damage from acetaminophen doesn’t always hurt at first. But if you start feeling any of these symptoms within 24 to 72 hours after taking the medication, get help immediately:
- Nausea or vomiting
- Loss of appetite
- Dark urine
- Clay-colored stools
- Jaundice (yellow skin or eyes)
- Pain in the upper right side of your belly
- Extreme tiredness
These aren’t “wait and see” symptoms. If you’ve taken acetaminophen and notice even one of these, go to the ER. The antidote - N-acetylcysteine (NAC) - works best if given within 8 hours of overdose. After 16 hours, it’s much less effective.
What About People With Liver Disease?
If you have hepatitis, cirrhosis, or fatty liver disease, acetaminophen isn’t automatically off-limits. But you need to be extra careful. The Veterans Affairs Hepatitis Resource Center says you can safely take up to 2,000 mg per day - that’s four 500 mg tablets - if you don’t drink alcohol. But many doctors recommend staying even lower, at 1,500 mg, especially if you’re older or have other health issues.
And never, ever take NSAIDs if you have advanced liver disease. They’re harder on your kidneys, and when your kidneys fail, your liver gets even more stressed. It’s a dangerous cycle.
Future Solutions Are Coming
Scientists are working on better ways to manage pain without hurting the liver. New drugs are being tested that don’t rely on liver metabolism at all. Genetic testing is now available to find out if you have a variant in your genes that makes you more sensitive to acetaminophen. Companies like 23andMe offer this as part of their health reports. If you’ve had liver problems before, it might be worth checking.
Also, the FDA has started requiring clearer warning labels on all OTC products. The front of the box now says “LIVER WARNING” in big letters. That’s helping. A 2023 study found that since these labels were added, unintentional overdoses dropped by 21%.
Final Rule: When in Doubt, Skip It
There’s no shame in skipping a pain reliever. If you’re not sure whether it’s safe, don’t take it. Talk to your pharmacist. Ask your doctor. Use a pain diary to track what you take and when. There are non-drug options that work - heat, rest, movement, massage. And if you’re managing chronic pain, physical therapy or cognitive behavioral therapy might be more effective than pills anyway.
Your liver doesn’t scream when it’s hurt. It just stops working. By the time you feel sick, it might be too late. Be smarter than the label. Know your dose. Know your risks. And never assume that because it’s sold over the counter, it’s harmless.
Can I take acetaminophen if I drink alcohol occasionally?
No, not safely. Even one drink a day can make your liver more vulnerable to acetaminophen damage. The safe daily limit drops from 4,000 mg to about 2,000 mg - and some experts say it’s safer to avoid it completely if you drink regularly. If you’re having a drink, skip the Tylenol. Use a cold compress or rest instead.
Is Tylenol safer than ibuprofen for my liver?
Tylenol (acetaminophen) is the main cause of drug-induced liver injury, but ibuprofen and other NSAIDs rarely cause liver damage. However, NSAIDs can harm your kidneys and stomach, especially if you have liver disease. For people with healthy livers and no stomach or kidney issues, both can be used carefully. But if you have liver disease, acetaminophen at low doses (≤2,000 mg) is often still preferred over NSAIDs.
How do I know if a cold medicine has acetaminophen?
Look for these names on the label: acetaminophen, APAP, or paracetamol. Cold and flu medicines like NyQuil, DayQuil, TheraFlu, and Zicam often contain it. If the product treats pain or fever, it likely has acetaminophen. Always read the “Active Ingredients” section - don’t just rely on the brand name.
Can I take acetaminophen if I have fatty liver disease?
Yes, but only at low doses - no more than 2,000 mg per day, and never with alcohol. Fatty liver means your liver is already working harder. Adding acetaminophen on top can push it over the edge. Talk to your doctor about alternatives like physical therapy, weight management, or topical pain relievers.
What should I do if I think I took too much acetaminophen?
Don’t wait for symptoms. Call poison control or go to the ER immediately. The antidote, N-acetylcysteine (NAC), works best within 8 hours of overdose. Even if you feel fine, liver damage can be silent at first. Waiting until you’re nauseous or yellow can be too late. It’s better to be safe than sorry.
Are there pain relievers that don’t affect the liver at all?
Topical NSAIDs like diclofenac gel or lidocaine patches don’t enter your bloodstream in large amounts, so they’re much safer for the liver. Other non-drug options include heat therapy, massage, physical therapy, acupuncture, and cognitive behavioral therapy. These don’t just mask pain - they help your body heal.
Can genetic testing tell me if I’m at higher risk for liver damage from acetaminophen?
Yes. Some people have genetic variations in the enzymes that break down acetaminophen. These variations can make them more likely to build up toxic levels even at normal doses. Companies like 23andMe now include this in their health reports. If you’ve had unexplained liver issues or family history of liver disease, genetic testing could help you avoid future risks.
