IPF Drug Comparison Tool
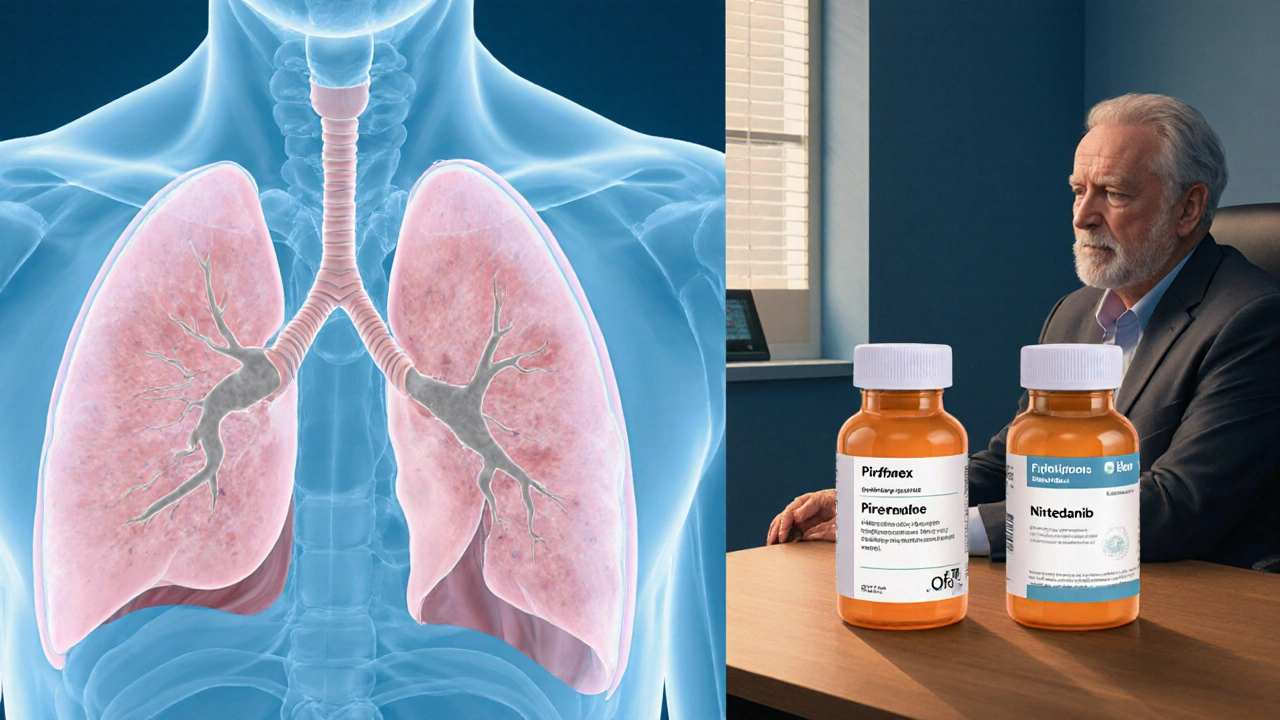
Pirfenex (Pirfenidone)
Mechanism: Inhibits TGF-β-driven fibroblast activity
Dosing: 801 mg × 3 times daily (titrated)
Primary Side Effects:
- Nausea
- Photosensitivity rash
- Liver enzyme elevation
FVC Decline Reduction: ~30%
Annual Cost (US): ≈ $12,000
Nintedanib (Ofev)
Mechanism: Blocks VEGF, PDGF, FGF receptors
Dosing: 150 mg × 2 times daily
Primary Side Effects:
- Diarrhea
- Nausea
- Liver enzyme elevation
FVC Decline Reduction: ~24%
Annual Cost (US): ≈ $14,000
Lung-function trajectory: Both drugs slow decline, but adherence to dosing may tip the balance.
Gastrointestinal tolerance: Patients with severe diarrhea may prefer Pirfenex; those who are photosensitive should avoid Pirfenex.
Liver health: Baseline ALT/AST >2× ULN suggests starting with the drug that has a milder hepatic profile – generally Nintedanib.
Insurance & cost: Check formularies; sometimes one drug is on a preferred tier.
Convenience: Three daily pills versus two can affect adherence, especially for older adults.
Recommended Approach
When you or a loved one are diagnosed with idiopathic pulmonary fibrosis (IPF), the biggest question becomes - which drug will slow the scar tissue and keep lungs working longer? Pirfenex is the brand name for pirfenidone, an oral antifibrotic approved in the US in 2014. It’s often mentioned alongside Nintedanib, the other FDA‑approved option. This article breaks down how they differ, what alternatives exist, and how to pick the right regimen for you.
Key Takeaways
- Pirfenex and Nintedanib are the only two drugs specifically approved for IPF.
- Pirfenex works by reducing fibroblast activity; Nintedanib blocks multiple growth‑factor receptors.
- Side‑effect profiles are distinct: Pirfenex commonly causes nausea and photosensitivity, while Nintedanib often leads to diarrhea.
- Costs vary by region and insurance; in South Africa, both can exceed R30000 per year.
- Choosing a therapy hinges on lung‑function decline rate, comorbidities, and personal tolerance for side effects.
What is Pirfenex (pirfenidone)?
Pirfenex (pirfenidone) is a small‑molecule oral drug that targets the fibrotic pathway in the lungs. Approved by the U.S. Food and Drug Administration (FDA) for adults with mild‑to‑moderate IPF, it is taken three times daily with meals to reduce gastrointestinal upset.
How Pirfenex Works
Pirfenex inhibits transforming growth factor‑beta (TGF‑β) signaling and reduces fibroblast proliferation. In simple terms, it slows the conversion of normal lung tissue into stiff scar tissue. Clinical trials showed a roughly 30% reduction in the annual decline of forced vital capacity (FVC), the standard measure of lung function.
Dosing & Administration
Typical titration starts at 267mg three times a day for the first week, then 534mg three times a day in week2, and finally 801mg three times a day from week3 onward. The dose may be reduced if liver enzymes rise or if severe nausea persists.
Typical Side‑Effects
Most patients experience mild to moderate nausea, loss of appetite, and a distinct photosensitivity rash. Liver‑function tests (ALT, AST) should be monitored every month for the first six months because hepatic injury occurs in roughly 5% of users.
Cost Considerations
Price varies by market. In the United States, the average wholesale price is about $12000 per year; in South Africa, the quoted price per pack can reach R1800, translating to roughly R35000 annually. Insurance coverage is inconsistent, making out‑of‑pocket expense a key decision factor.
Alternative Approved Drug: Nintedanib
Nintedanib (brand name Ofev) is a tyrosine‑kinase inhibitor that blocks vascular endothelial growth factor (VEGF), platelet‑derived growth factor (PDGF), and fibroblast growth factor (FGF) receptors. Like Pirfenex, it was approved by the FDA in 2014.
How Nintedanib Works
By simultaneously inhibiting three pathways that drive fibroblast proliferation, Nintedanib reduces the rate of FVC decline by about 24% in pivotal trials. It is taken twice daily with food.
Side‑Effects of Nintedanib
The most common adverse event is diarrhea, affecting up to 70% of patients; anti‑diarrheal medication is often prescribed alongside. Liver enzyme elevations are also observed, though less frequently than with Pirfenex.
Cost of Nintedanib
Annual cost sits near $14000 in the US and roughly R38000 in South Africa. Some health‑plan formularies place it on a higher tier, increasing co‑pay requirements.
Other Emerging Options
Beyond the two approved agents, several drugs are in PhaseIII trials:
- Pamrevlumab - an anti‑connective tissue growth factor antibody.
- PRM-151 - recombinant human pentraxin‑2.
- BMS‑986020 - an integrin inhibitor (development paused due to safety concerns).
These are not yet available for routine prescribing but signal that the therapeutic landscape may broaden in the next few years.
Direct Comparison
| Attribute | Pirfenex (pirfenidone) | Nintedanib (Ofev) |
|---|---|---|
| Mechanism | Inhibits TGF‑β‑driven fibroblast activity | Blocks VEGF, PDGF, FGF receptors |
| Dosing schedule | 801mg×3times daily (titrated) | 150mg×2times daily |
| Primary side‑effects | Nausea, photosensitivity, liver enzyme rise | Diarrhea, nausea, liver enzyme rise |
| FVC decline reduction | ~30% (CAPACITY & ASCEND trials) | ~24% (INPULSIS trials) |
| Approval year (US) | 2014 | 2014 |
| Annual cost (US) | ≈ $12000 | ≈ $14000 |
Choosing the Right Therapy
There is no one‑size‑fits‑all answer. Consider these decision points:
- Lung‑function trajectory: If the patient loses >10% FVC per year, both drugs slow decline, but adherence to dosing may tip the balance.
- Gastro‑intestinal tolerance: Patients with a history of severe diarrhea may prefer Pirfenex; those who are photosensitive should avoid Pirfenex.
- Liver health: Baseline ALT/AST >2× ULN suggests starting with the drug that has a milder hepatic profile - generally Nintedanib.
- Insurance & out‑of‑pocket cost: Check formularies; sometimes one drug is on a preferred tier.
- Convenience: Three daily pills versus two can affect adherence, especially for older adults.
Discuss each factor with a pulmonologist. Many clinicians start with Pirfenex, monitor liver enzymes, and switch if gastrointestinal side effects dominate.
Managing Side‑Effects
Proactive strategies improve continuation rates:
- For Pirfenex nausea: Take each dose with a full meal, consider anti‑emetics like ondansetron, and use a proton‑pump inhibitor if reflux is present.
- For photosensitivity: Apply broad‑spectrum sunscreen (SPF30+), wear UV‑blocking clothing, and limit direct sun exposure during peak hours.
- For Nintedanib diarrhea: Initiate loperamide at the first sign of loose stools, stay hydrated, and keep a low‑fat diet.
Regular blood work (ALT, AST, bilirubin) every 4‑6weeks for the first 6months is a simple way to catch hepatic issues early.
Future Outlook
Research is moving toward combination therapy-using both Pirfenex and Nintedanib together. Early‑phase studies suggest additive reduction in FVC decline, but safety data are still pending. Until larger trials confirm benefits, doctors stick to monotherapy.
Frequently Asked Questions
Can I switch from Pirfenex to Nintedanib?
Yes. Most physicians will taper Pirfenex over a week, then start Nintedanib at the standard 150mg twice daily. Monitoring liver enzymes during the transition is essential.
Is one drug better for severe IPF?
Both drugs have shown benefit in mild‑to‑moderate disease; data in advanced disease are limited. In practice, clinicians choose based on side‑effect tolerance and comorbidities rather than severity alone.
Do I need regular scans while on Pirfenex?
Routine high‑resolution CT scans are not required every year; a baseline scan followed by one at 12‑month intervals is typical, unless symptoms worsen.
Can I take Pirfenex if I have liver disease?
Caution is advised. If your ALT/AST are already >2×ULN, doctors usually start with a reduced dose or prefer Nintedanib, which may have a milder hepatic impact.
Are there lifestyle changes that boost drug effectiveness?
Maintaining a healthy weight, quitting smoking, and staying physically active can preserve lung capacity longer, complementing either drug’s antifibrotic effect.
Bottom Line
For anyone wrestling with IPF, the Pirfenex comparison boils down to side‑effect tolerance, dosing convenience, and cost. Nintedanib offers a twice‑daily regimen with a different GI profile, while Pirfenex demands three daily doses but may suit patients who dislike frequent loose stools. Talk to a specialist, weigh the pros and cons outlined above, and keep a close eye on liver labs-your choice could add precious months of breathing easier.
Pirfenex seems like a solid option if you can handle the pills three times a day.
While both Pirfenex and Nintedanib demonstrate efficacy in slowing FVC decline, the decision should hinge upon individual tolerance to gastrointestinal side effects, hepatic function, and insurance coverage, all of which merit careful consideration.
In clinical practice the choice between Pirfenex and Nintedanib often starts with a review of the patient’s baseline liver enzymes; elevated ALT or AST may sway the clinician toward Nintedanib, which historically shows a milder hepatic profile. Equally important is the gastrointestinal tolerance: patients with chronic diarrhea usually find Nintedanib’s twice‑daily dosing more manageable, whereas those who are photosensitive might benefit from Pirfenex’s thrice‑daily schedule with diligent sun protection. Cost remains a decisive factor, with Nintedanib averaging a higher annual price in the United States, though formulary placement can invert that relationship. Adherence is another practical consideration; older adults or those on complex medication regimens often struggle with three daily doses, potentially reducing the real‑world effectiveness of Pirfenex. Ultimately, a shared decision‑making conversation that weighs these variables will produce the most personalized therapeutic plan.
I hear you on the adherence issue – three pills a day can feel like a marathon, especially if you’re already juggling inhalers and supplements. A good trick is to pair each dose with a regular mealtime; it not only masks the nausea but also creates a routine you’re less likely to forget.
When you start digging into the literature, a pattern emerges that is hard to ignore: both Pirfenex and Nintedanib have proven, in randomized controlled trials, to slow the decline of forced vital capacity by roughly a quarter to a third, yet they achieve this through entirely different molecular pathways.
The first red flag many patients overlook is the hidden cost of surveillance – weekly liver function tests for the first six months can become a logistical nightmare, especially for those living in remote areas.
Add to that the fact that photosensitivity, while often dismissed as a mild rash, can lead to severe burns if patients are not educated about sunscreen use and UV avoidance.
Conversely, the diarrhea associated with Nintedanib is not merely an inconvenience; chronic fluid loss can precipitate electrolyte imbalances, exacerbating cardiovascular comorbidities that are common in the IPF population.
There is also the psychological burden of taking medication that reminds you daily of a chronic, progressive disease, which can affect adherence in ways that are difficult to quantify.
Insurance formularies, as you know, are a moving target – a drug that is tier‑1 today might be bumped to tier‑3 next quarter, forcing a sudden out‑of‑pocket spike that many patients cannot absorb.
From a pharmacoeconomic standpoint, the incremental cost‑effectiveness ratio of Pirfenex versus Nintedanib varies wildly across healthcare systems, suggesting that a one‑size‑fits‑all recommendation is fundamentally flawed.
Moreover, emerging data on combination therapy hint at additive benefits, but the safety profile of simultaneous antifibrotic use remains largely uncharted territory.
Patients with pre‑existing liver disease should not be cavalier; even mild elevations in transaminases can herald a cascade of hepatic injury that may necessitate abrupt drug cessation.
On the other hand, those with irritable bowel syndrome may find the diarrhea from Nintedanib intolerable, leading to dose reductions that diminish therapeutic effect.
Real‑world registries have shown that discontinuation rates hover around 30% for both agents, often citing adverse events rather than lack of efficacy.
In clinical settings where multidisciplinary teams are available, the integration of pulmonology, pharmacy, and nutrition services can mitigate many of these side‑effects through proactive counseling.
Anecdotally, patients who embrace lifestyle modifications-like low‑fat diets, regular light exercise, and smoking cessation-report a subjective sense of control that may amplify drug benefits.
Finally, the decision matrix is not static; as patients age or develop new comorbidities, the risk‑benefit calculus shifts, requiring periodic reassessment rather than a single, once‑and‑for‑all choice.
In summary, while both drugs are valuable tools in the IPF armamentarium, the optimal selection hinges on a mosaic of clinical, economic, and personal factors that only a nuanced, patient‑centered dialogue can resolve.
Yo, that’s a mountain of info – makes me wonder why pharma ain’t just drop a combo pill already.
Given the presented data, one might inquire whether the differential impact on hepatic enzymes could be quantified in a meta‑analysis, thereby offering a more precise risk stratification for patients with borderline liver function.
Nintedanib works well but watch the gut.
Yeah, the diarrhea can really throw you off your day‑to‑day routine if you’re not prepared.
Both meds have their pros and cons, so pick the one that matches your lifestyle and stick with it.
Don’t forget that the pharma giants love to hide the long‑term side effects; they’ll push whatever makes the biggest profit while we’re left dealing with hidden risks.
The debate over Pirfenex versus Nintedanib is nothing short of a theatrical showdown of science and greed
Let’s cut the drama – the truth is both drugs can help, and the best choice comes down to personal health factors, not conspiracies.
i think you should check the dosing schedule.
Well, duh, the dosing schedule is alrady on the label – if you cant read it, maybe read it again.
Stay hopeful folks! Whether you’re on Pirfenex or Nintedanib, keeping a positive mindset and staying on top of your appointments can make a big difference in quality of life.
Absolutely! 🌟 Embracing the journey with courage and curiosity can turn the tide – a little optimism 🌈 and diligent care go hand‑in‑hand with these therapies.