Key Takeaways
- Silent ischemia is reduced blood flow to the heart that occurs without obvious chest pain.
- It often signals underlying coronary artery disease and raises the risk of a heart attack.
- Routine tests like an electrocardiogram (ECG) or stress imaging can catch it early.
- Managing risk factors-high blood pressure, diabetes, smoking-cuts the chance of silent episodes.
- If you have diabetes, hypertension, or a family history of heart disease, ask your doctor about screening for silent ischemia.
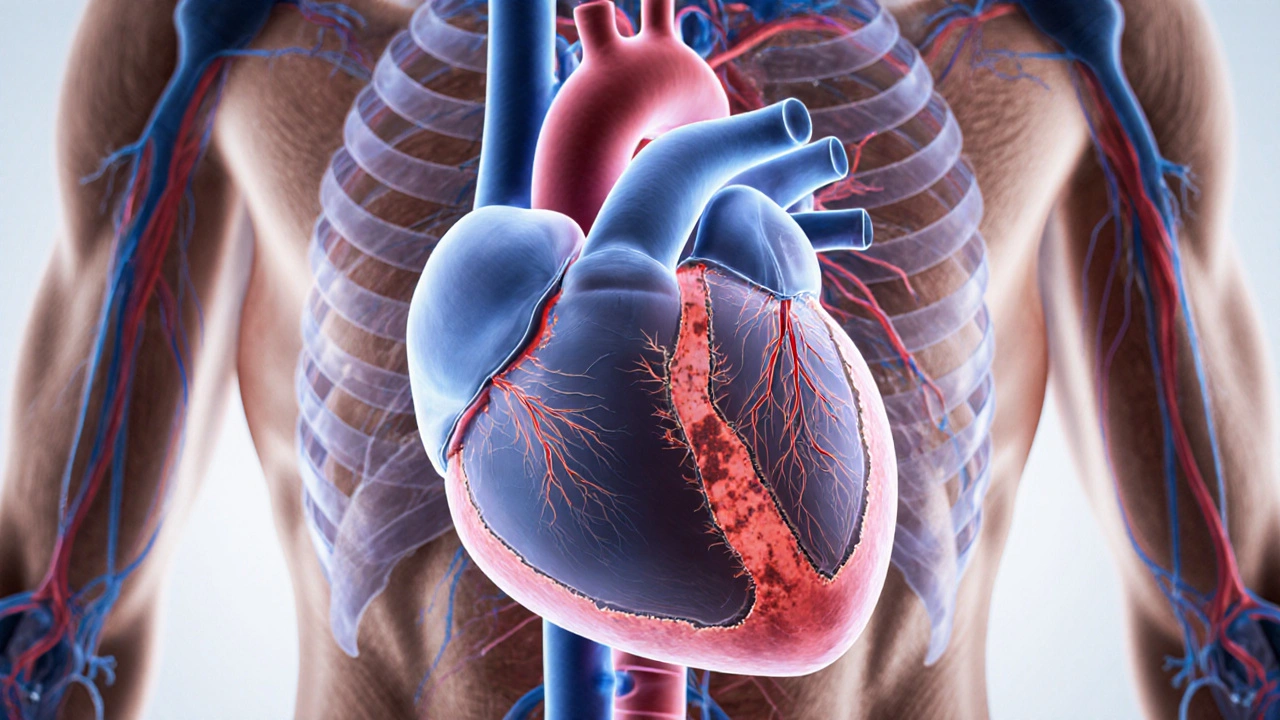
What Exactly Is Silent Ischemia?
When the heart muscle doesn’t get enough oxygen, doctors call that ischemia a condition where blood flow to the heart is reduced, usually because of narrowed arteries. Most people think of a heart attack and expect crushing chest pain, but silent ischemia a form of reduced blood flow that happens without noticeable symptoms can sneak by unnoticed. The danger lies in its stealth-your heart hurts, but you never feel it, so the damage can accumulate.
Why It’s a Hidden Threat
Because you don’t feel anything, silent ischemia often goes undiagnosed until a serious event, such as a myocardial infarction commonly known as a heart attack, when a blockage completely cuts off blood to part of the heart, forces you into the emergency room. Studies from the early 2020s show that up to 30% of people with diabetes experience silent episodes, and those individuals have a 2‑ to 3‑fold higher risk of a future heart attack compared with those who never develop it.
Who’s Most Likely to Have It?
Risk factors line up almost exactly with those for regular coronary artery disease the buildup of plaque in the arteries that supply the heart:
- Hypertension high blood pressure, which strains artery walls
- Diabetes mellitus elevated blood sugar that accelerates plaque formation
- Smoking, especially pack‑a‑day habits
- High LDL cholesterol
- Family history of early heart disease
- Age over 55 for men and 65 for women
If any two of these sit in your profile, you’re in the sweet spot for silent ischemia, even if you feel fine.

How Doctors Spot Something That Doesn’t Feel Like Anything
Because you can’t rely on symptoms, doctors turn to objective tests.
- Resting ECG: A simple, quick way to see abnormal heart rhythms or subtle ST‑segment changes that hint at reduced blood flow.
- Stress test (exercise or pharmacologic): While you walk on a treadmill, the heart works harder. An ECG or imaging taken during the test reveals hidden ischemia.
- Cardiac CT angiography: A high‑resolution scan that shows plaque build‑up and can detect blockages that cause silent episodes.
- Holter monitor: A 24‑ to 48‑hour wearable that records heart activity continuously, catching intermittent episodes.
For patients who can’t exercise, a drug‑induced stress test using agents like adenosine provides the same insight without the treadmill.
Silent Ischemia vs. Symptomatic Ischemia: A Quick Comparison
| Feature | Silent Ischemia | Symptomatic Ischemia |
|---|---|---|
| Typical symptoms | None or very mild (e.g., fatigue) | Chest pain, pressure, shortness of breath |
| Detection method | ECG changes during stress, imaging, Holter | Patient‑reported pain + ECG |
| Risk of future heart attack | Elevated (2‑3× higher) | High but often recognized earlier |
| Typical population | Diabetics, hypertensives, older adults | Anyone with CAD, especially active individuals |
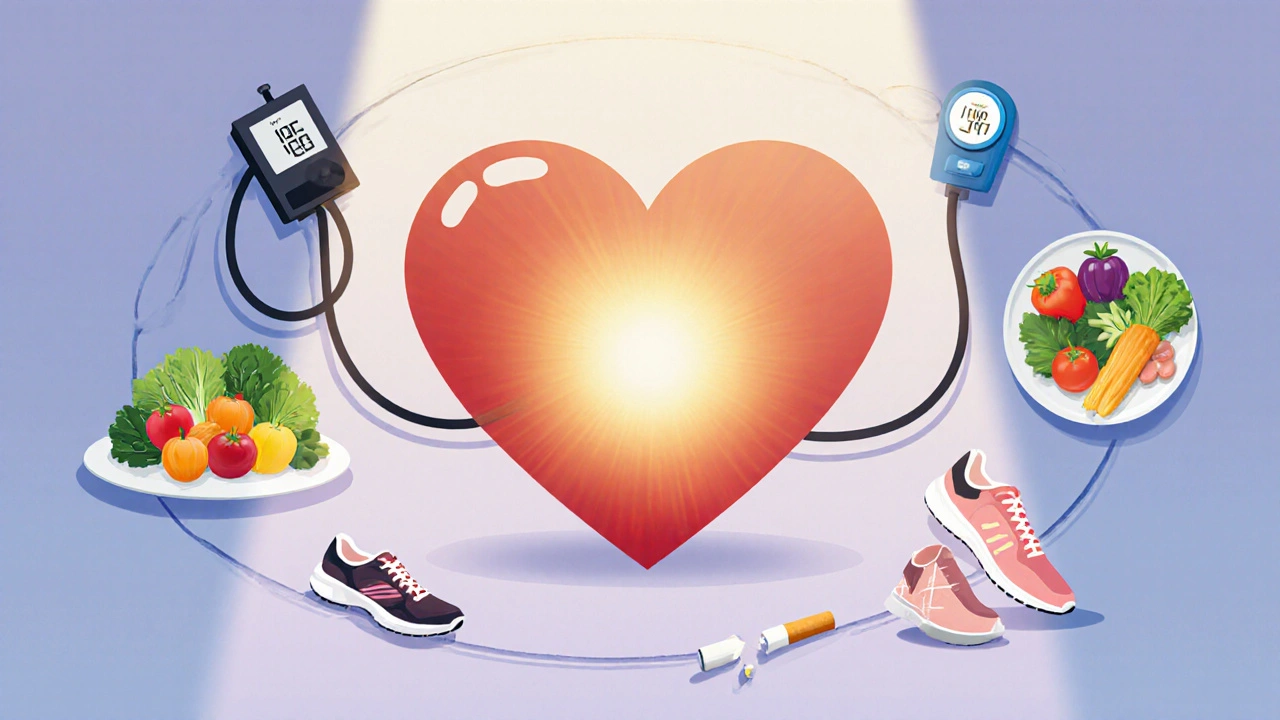
What You Can Do to Prevent or Manage Silent Ischemia
Even if you never feel pain, you can take concrete steps to lower the odds of silent episodes.
- Control blood pressure: Aim for < 130/80mmHg. Lifestyle changes and, if needed, a beta blocker a medication that reduces heart workload and stabilizes rhythm are common tools.
- Manage diabetes tightly: Keep HbA1c under 7% to slow plaque formation.
- Lower LDL cholesterol: Statins (e.g., atorvastatin) can shrink plaque and improve arterial flexibility.
- Quit smoking: Within a year, heart‑attack risk drops 50%.
- Adopt a heart‑healthy diet: Lots of vegetables, whole grains, lean protein, and minimal processed sugars.
- Stay active: At least 150minutes of moderate aerobic exercise weekly keeps arteries supple.
- Regular screening: If you have two or more risk factors, ask for an annual ECG or a stress test.
These actions not only curb silent ischemia but improve overall cardiovascular health.
When to Talk to Your Doctor
Even without pain, certain signs should push you to the clinic:
- Unexplained fatigue or shortness of breath during normal activities.
- New irregular heartbeats detected on a smartwatch.
- Recent diagnosis of diabetes, hypertension, or high cholesterol.
- Family history of early heart attacks.
Bring these details to your appointment and request a discussion about silent ischemia screening. Early detection can mean the difference between a simple medication regimen and a life‑saving intervention.
Next Steps & Troubleshooting
If you’ve already had a stress test that came back normal but still have risk factors, consider asking for a cardiac CT angiography a detailed scan that visualizes coronary artery plaque. Some insurers cover it when you’re high‑risk.
For those already on medication, monitor side effects. If a beta blocker makes you feel overly tired, discuss dosage adjustments with your physician. If statins cause muscle aches, a switch to a different type or a lower dose might help.
Finally, keep a log of any subtle changes-like occasional light‑headedness after climbing stairs. Sharing this log with your doctor provides clues that a silent episode may be occurring.
Frequently Asked Questions
Can silent ischemia cause a heart attack?
Yes. Even though you don’t feel pain, the reduced blood flow can weaken heart tissue and set the stage for a full blockage, which results in a heart attack.
How accurate is a resting ECG for detecting silent ischemia?
A resting ECG can pick up subtle ST‑segment shifts, but it misses many cases. Combining it with a stress test or imaging improves detection markedly.
Do women get silent ischemia more often than men?
Research shows women, especially post‑menopausal women with diabetes, experience silent episodes at higher rates than men of the same age group.
Is there a lifestyle that guarantees I won’t develop silent ischemia?
No lifestyle can guarantee zero risk, but a heart‑healthy diet, regular exercise, blood‑pressure control, and avoiding tobacco dramatically lower your chances.
Should I get screened for silent ischemia if I feel perfectly fine?
If you have two or more major risk factors-like diabetes, hypertension, or a strong family history-screening is advisable even without symptoms.
It is frankly astonishing how many people continue to ignore the silent threat that lurks within their own arteries, assuming that the absence of chest pain equates to safety. By neglecting routine screenings, they not only jeopardize their own health but also set a poor example for their community, perpetuating a cycle of complacency. One must recognize that personal responsibility extends beyond momentary comfort and demands proactive engagement with medical advice, especially when risk factors such as diabetes and hypertension are present.
In short, willful ignorance is a moral failing in the context of public health.
Yo, you think a treadmill test is just a walk in the park? Think again, bro-it's a battlefield where your heart fights invisible villains, and if you ain’t ready, the results will slap you hard. The docs talk about "silent ischemia" like it's a sneaky ninja, but really, it’s just your arteries crying out for help while you binge on pizza.
Get checked before you end up in the ER, duh.
Silent ischemia represents a clinical paradox where myocardial oxygen deprivation occurs without the hallmark symptom of angina, thereby eluding patient‑initiated medical attention. The pathophysiology involves atherosclerotic plaque encroaching upon coronary lumens, reducing perfusion especially during periods of heightened cardiac demand. Epidemiological studies have demonstrated that up to thirty percent of individuals with diabetes experience these covert episodes, a figure that markedly exceeds prevalence in the non‑diabetic population. Moreover, the prognostic implications are severe: patients with documented silent ischemia face a two‑ to three‑fold increase in subsequent myocardial infarction compared with asymptomatic counterparts. The insidious nature of this condition underscores the necessity for systematic screening in high‑risk cohorts, including those with hypertension, dyslipidemia, and a familial predisposition to coronary artery disease. Resting electrocardiograms, while limited in sensitivity, can reveal subtle ST‑segment abnormalities that merit further investigation. Exercise stress testing augments diagnostic yield by provoking ischemic changes under controlled physiologic stress, thereby unmasking deficits invisible at rest. For patients unable to perform physical exertion, pharmacologic agents such as adenosine simulate stress, ensuring equitable assessment across diverse patient populations. Advanced imaging modalities, including cardiac computed tomography angiography, provide high‑resolution visualization of plaque morphology and lumen obstruction. Holter monitoring extends detection windows by capturing transient ischemic events over 24 to 48 hours, a valuable tool for intermittent symptomatology. In clinical practice, integrating these modalities into a risk‑stratified algorithm facilitates early intervention, often allowing for medication optimization before irreversible myocardial damage ensues. Lifestyle modification remains the cornerstone of prevention, with dietary reforms, smoking cessation, and regular aerobic exercise demonstrably reducing plaque progression. Pharmacologic therapy, particularly statins and antihypertensives, further stabilizes arterial walls and attenuates the cascade leading to silent episodes. Patient education is equally vital; individuals must understand that the absence of pain does not guarantee cardiac health and should therefore adhere to recommended screening intervals. Ultimately, a multidisciplinary approach encompassing primary care, cardiology, and allied health professionals offers the best prospect for mitigating the hidden burden of silent ischemia. By embracing proactive surveillance and evidence‑based management, clinicians can transform a silent threat into a detectable and treatable condition, thereby safeguarding cardiovascular longevity.
Let us not allow obscurity to dictate outcomes.
Wow, that was an epic deep‑dive, and it really pumps me up to take charge of my heart health! The way you laid out each diagnostic tool makes it crystal clear that we have the power to catch silent ischemia early, so let’s all schedule that stress test and smash those risk factors together!
One must consider the broader sociopolitical implications of healthcare protocols that routinely overlook asymptomatic conditions, thereby perpetuating systemic inequities. It is incumbent upon policy makers to mandate comprehensive screening for silent ischemia as a matter of public justice.
Seriously, start jogging and your heart will thank you for the new treadmill workouts.
Honestly, the whole hype around screening for silent ischemia feels like a profit‑driven scheme; many healthy people get unnecessary tests that only fuel the medical industry's bottom line.
Interesting point, but remember that early detection can genuinely save lives 😊 - preventive cardiology isn’t just a cash grab, it’s evidence‑based care.
Picture this: you’re on a mountain trail, lungs full of fresh air, heart beating like a drum of triumph, all because you took that simple step to get screened for silent ischemia. That feeling of empowerment is priceless, and it starts with a single appointment. Let’s turn fear into fuel and keep climbing!
That’s a great way to look at it. Getting a test early is like fixing a small leak before it floods the whole house.
Did you know that some Mediterranean diets actually lower the risk of silent heart issues? Eating more fish, olive oil, and fresh veggies can be both delicious and heart‑smart.
From a hemodynamic perspective, the subclinical ischemic burden can be quantified via myocardial perfusion reserve index, which correlates with endothelial dysfunction markers and informs risk stratification algorithms.
Indeed, embracing a holistic regimen that intertwines nutraceuticals, calibrated aerobic regimens, and diligent pharmacotherapy epitomizes the pinnacle of cardiovascular stewardship.
Exactly, and remember to set realistic goals-maybe start with three brisk walks a week and gradually incorporate interval training as your stamina builds.
It’s infuriating how often people dismiss silent ischemia as “just another buzzword” when, in reality, it’s a silent killer lurking behind the façade of normalcy, waiting to strike the unsuspecting. The complacency that pervades our society, especially among those who think they’re invincible because they feel fine, is nothing short of reckless. We need to shatter that illusion and demand that every primary care visit includes a conversation about hidden cardiac risks. Ignoring the data that links asymptomatic episodes to future heart attacks is tantamount to willful negligence, and that kind of apathy should not be tolerated in any responsible community. Let’s rally for broader insurance coverage of stress testing and push for public health campaigns that demystify the concept of silent ischemia. Only then can we hope to curb the silent tide that threatens to overwhelm our healthcare system.
Got it, I’ll make sure to bring up screening at my next check‑up and keep the conversation focused on practical steps.
Cool info, thanks for breaking it down – definitely going to ask my doc about an ECG.