Why Steroid Tapering Isn’t Just a Suggestion - It’s a Lifesaver
If you’ve been on prednisone or another glucocorticoid for more than three weeks, stopping it cold turkey isn’t just risky - it can land you in the hospital. Your body doesn’t produce enough natural cortisol anymore because the steroid has told your adrenal glands to take a break. When you suddenly cut the drug, your body doesn’t know how to restart. That’s when fatigue hits hard, your blood pressure drops, and your autoimmune disease comes roaring back - sometimes worse than before.
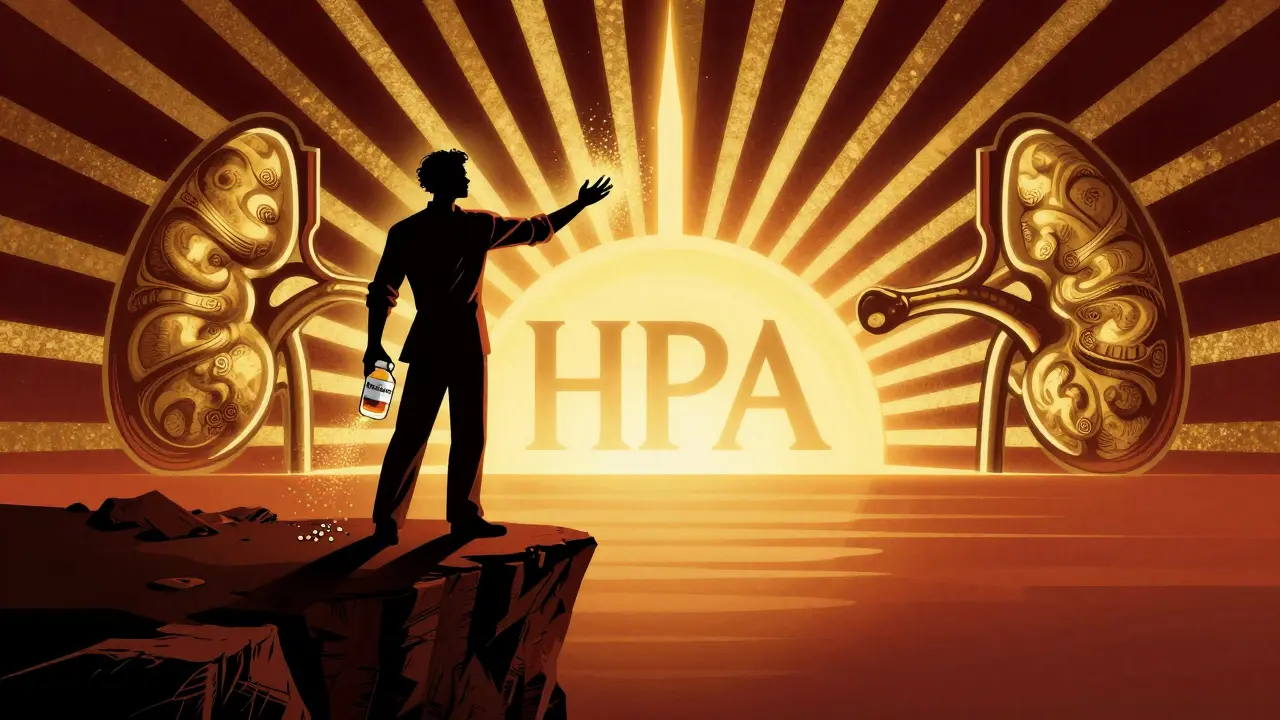
Steroid tapering isn’t about being lazy or avoiding the end of treatment. It’s about giving your body time to wake up its own cortisol production. The HPA axis - your hypothalamus, pituitary, and adrenal glands - needs weeks or even months to recover. Rushing this process is like yanking the plug on a generator that’s still warming up.
How Fast Should You Taper? It Depends on Your History
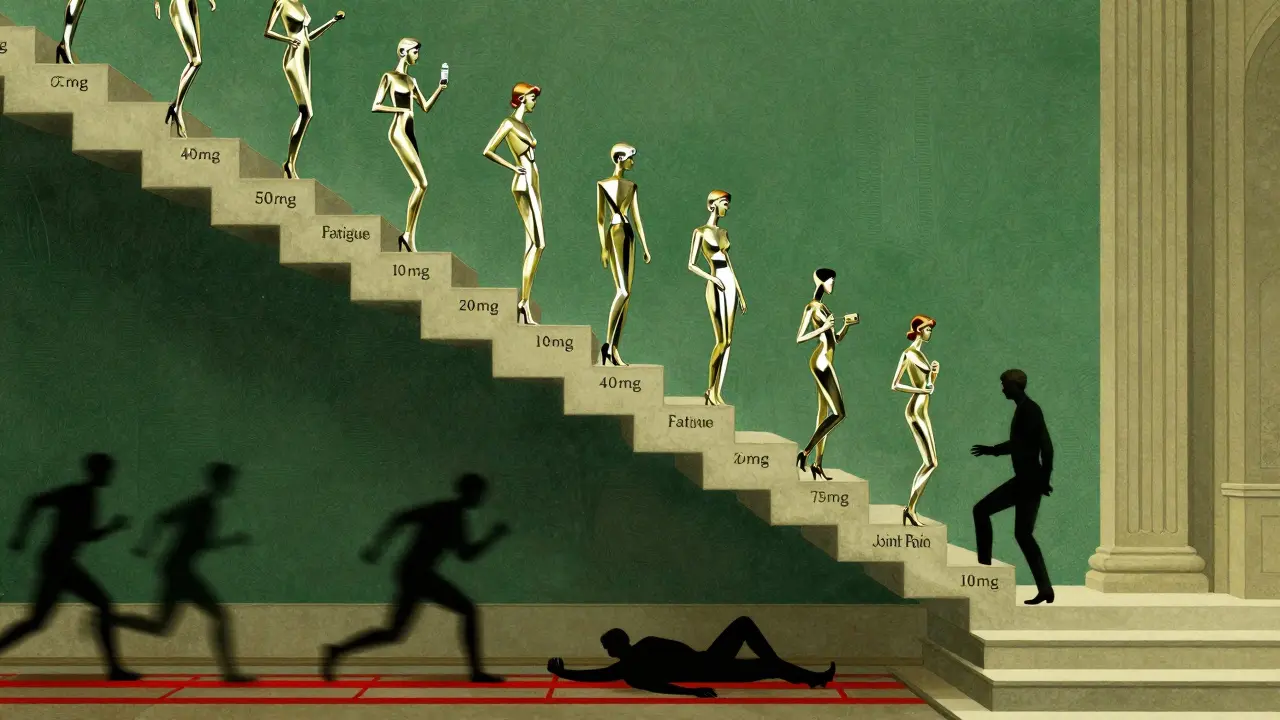
There’s no one-size-fits-all schedule. If you were on high-dose steroids (over 40 mg of prednisone daily) for only a few weeks, you might be able to taper off in 10 to 14 days. But if you’ve been on 10 mg or more for six months or longer? Plan for 3 to 6 months. The longer you’ve been on steroids, the slower the taper must be.
Here’s what most doctors follow:
- Initial rapid taper: Drop by 5-10 mg every week until you hit 20 mg/day. This is safe because your body still has some cortisol production left.
- Gradual taper: Once you’re at 20 mg, reduce by 5 mg every two weeks until you reach 10 mg. This is where many people start feeling off - fatigue, joint pain, brain fog.
- Slow taper: From 10 mg down to 5 mg, drop by 2.5 mg every two weeks. Then go from 5 mg to 2.5 mg over two to four weeks. After that, it’s often 2.5 mg every other day, then stop.
Some doctors switch patients from prednisone to hydrocortisone near the end. Hydrocortisone is closer to natural cortisol and has a shorter half-life. But here’s the catch: most studies show you don’t need to switch. You can taper prednisone directly. The switch adds complexity without clear benefit for most people.
What Happens When You Taper Too Fast?
Withdrawal symptoms aren’t just ‘feeling tired.’ They’re your body screaming for cortisol. Common signs include:
- Extreme fatigue that doesn’t improve with sleep
- Muscle and joint pain that feels like arthritis flare
- Nausea, dizziness, or low blood pressure
- Insomnia or mood swings
- Loss of appetite or weight loss
And if you ignore these signs? Your autoimmune disease - whether it’s rheumatoid arthritis, lupus, or inflammatory bowel disease - can flare badly. In some cases, you’ll end up needing more steroids than you started with. That’s the worst-case scenario: a vicious cycle where tapering fails, the disease returns, and you’re back on high doses.
One patient in a WebMD survey dropped from 7.5 mg to 5 mg too fast and got severe joint pain. She had to hold at 7.5 mg for two weeks before trying again. That’s not failure - that’s smart pacing.
How to Spot a Flare vs. Withdrawal
This is where things get tricky. Joint pain from withdrawal feels similar to a disease flare. So how do you tell the difference?
Withdrawal symptoms tend to be more generalized: whole-body fatigue, achiness, mood changes. A true flare is usually localized - say, swollen knees in rheumatoid arthritis, or bloody diarrhea in ulcerative colitis. Flares also come with lab markers: elevated CRP, ESR, or specific autoantibodies.
If you’re unsure, don’t guess. Call your doctor. A simple blood test can check your inflammation levels. If your markers are normal but you still feel awful, it’s likely withdrawal. If your markers are up? You might need to pause the taper.
What to Do When Withdrawal Hits
You’re not powerless when symptoms show up. Here’s what works:
- Movement, not rest: Bed rest makes stiffness worse. Gentle walks - even 10 minutes twice a day - reduce joint pain by 57% compared to staying still.
- Warm water therapy: Swimming or soaking in a warm bath eases muscle tension and improves circulation. Many patients report relief within days.
- 10-minute daily meditation: Stress worsens withdrawal. Studies show daily mindfulness cuts symptom severity by 43%.
- Hold the dose: If symptoms hit hard, pause the taper for 1-2 weeks. Stay at the same dose until you feel stable. Then try reducing again, maybe by smaller steps.
There’s no shame in slowing down. Tapering isn’t a race. It’s a recovery process.
Never Skip the ‘Sick Day Rules’
Even after you stop steroids, your adrenal glands might still be sleeping. If you get sick - flu, infection, surgery, even a bad dental procedure - your body needs extra cortisol to handle the stress.
That’s where ‘sick day rules’ come in. If you’re ill, double your last steroid dose for 2-3 days. If you’re vomiting or can’t keep pills down, you may need an emergency injection. Many patients don’t know this - and that’s why 18% of ER visits after tapering are due to adrenal crisis from untreated illness.
Always carry a steroid alert card. It says you’ve been on long-term steroids and may need emergency hydrocortisone. Keep it in your wallet. Tell your family. Post it on your phone lock screen.
What About Testing Your Cortisol Levels?
Some doctors check your morning cortisol level to see if your adrenals are waking up. But here’s the truth: routine testing isn’t recommended for most people. The results can be misleading. Cortisol levels fluctuate. A single number doesn’t tell you if your HPA axis is truly recovered.
Testing is only useful if you’re having clear withdrawal symptoms and your doctor suspects adrenal insufficiency. Even then, it’s often followed by a stimulation test - where you get an injection of ACTH to see if your adrenals respond. That’s not done in regular clinics. It’s for specialists.
Don’t chase tests. Chase symptoms. If you feel better at a lower dose, keep going. If you feel worse, pause.
The Future of Steroid Tapering
Doctors are starting to move away from fixed schedules. Instead, they’re using disease activity to guide tapering. For example, if your rheumatoid arthritis is in remission (DAS28 score below 2.6), you can reduce faster. If inflammation markers are creeping up? Hold the taper.
New tools are helping too. Apps like the Prednisone Taper Assistant use AI to adjust your schedule based on how you’re feeling. In pilot studies, patients using it stuck to their plan 82% of the time - far better than paper schedules.
But here’s the bottom line: no app or blood test replaces good communication with your doctor. Tapering is a team effort.
What to Expect After You Stop
Even after you take your last pill, your body isn’t done healing. Full HPA axis recovery can take up to 18 months. During that time, you’re still at risk for adrenal crisis if you get seriously ill.
That’s why you need to stay alert. Don’t assume you’re ‘cured’ just because you’re off steroids. Keep your alert card. Know your sick day rules. Watch for fatigue or dizziness that doesn’t go away.
Many people feel better within weeks. Others take months. Both are normal. The goal isn’t to rush back to ‘normal’ - it’s to find a new, stable rhythm where your body can run on its own fuel again.
Final Thoughts: Patience Is Your Best Medicine
Steroid tapering isn’t about being perfect. It’s about being consistent. It’s about listening to your body. It’s about knowing when to push and when to pause.
You didn’t get sick overnight. You won’t recover overnight either. But if you stick to a smart, individualized plan - with your doctor’s support - you can get off steroids without losing control of your disease or your health.
The right taper doesn’t just avoid withdrawal. It gives you back your life - safely, steadily, and for good.
i read this and thought wow this is actually helpful but then i realized i forgot to take my prednisone this morning and now my back feels like its made of wet cardboard. oops.
people dont understand that this isnt about willpower. its about biology. your body got lazy because you gave it an easy way out. now its mad. and it should be. you cant just flip a switch and expect your adrenals to jump back to work like a lazy intern on monday morning.
i’ve been tapering for 14 months now and honestly? the hardest part wasn’t the physical stuff. it was the guilt. like, why do i feel so bad when i’m not even sick anymore? but this post nailed it - your body isn’t broken, it’s just relearning how to be itself again. slow is the only way. and yes, i still take warm baths daily. no shame in that.
this is why big pharma wants you to stay on these drugs forever. they make billions off your dependence. they don’t care if you’re in pain. they just want you to keep buying. wake up people. this isn’t medicine - it’s a trap.
wait so you’re telling me the government and doctors are lying about steroid tapering? because i read a study from 2003 that says cortisol recovery is mostly psychological. and now i’m suspicious of everything. also, my cat has been staring at me weirdly since i started tapering. coincidence?
i tapered too fast and ended up in the ER. they gave me a shot of hydrocortisone and looked at me like i was an idiot. which i was. but now i carry a little vial in my pocket like it’s my personal power ring. also, i yell at trees when i’m tired. it helps.
i dont know much about this stuff but i think its important to listen to your body. i used to think i had to push through everything but now i just take walks and drink water and try not to stress too much. also i think the warm bath thing is smart. my mom always said warm water fixes everything
The scientific consensus on HPA axis recovery remains robust, and the recommendation to taper gradually is supported by multiple randomized controlled trials, including the 2018 Cochrane Review on glucocorticoid withdrawal. Furthermore, the use of sick-day rules is not anecdotal but evidence-based, with a number needed to treat of 5.6 to prevent adrenal crisis in high-risk populations.
i cried when i finally got to 2.5mg. not because i was sad - because i was so tired of being tired. and then i went for a walk in the rain and it felt like the first time in years i was really alive. this post? it saved me. thank you. i’m still on my journey but now i know i’m not crazy for needing time.
It is imperative to underscore that the notion of 'tapering by feel' lacks empirical validation and may result in suboptimal clinical outcomes. While anecdotal reports of symptom relief are common, they are confounded by placebo effects and regression to the mean. Standardized, protocol-driven tapering schedules, aligned with disease activity metrics and serial cortisol assessments, remain the gold standard. Emotional narratives, however compelling, do not substitute for clinical rigor.