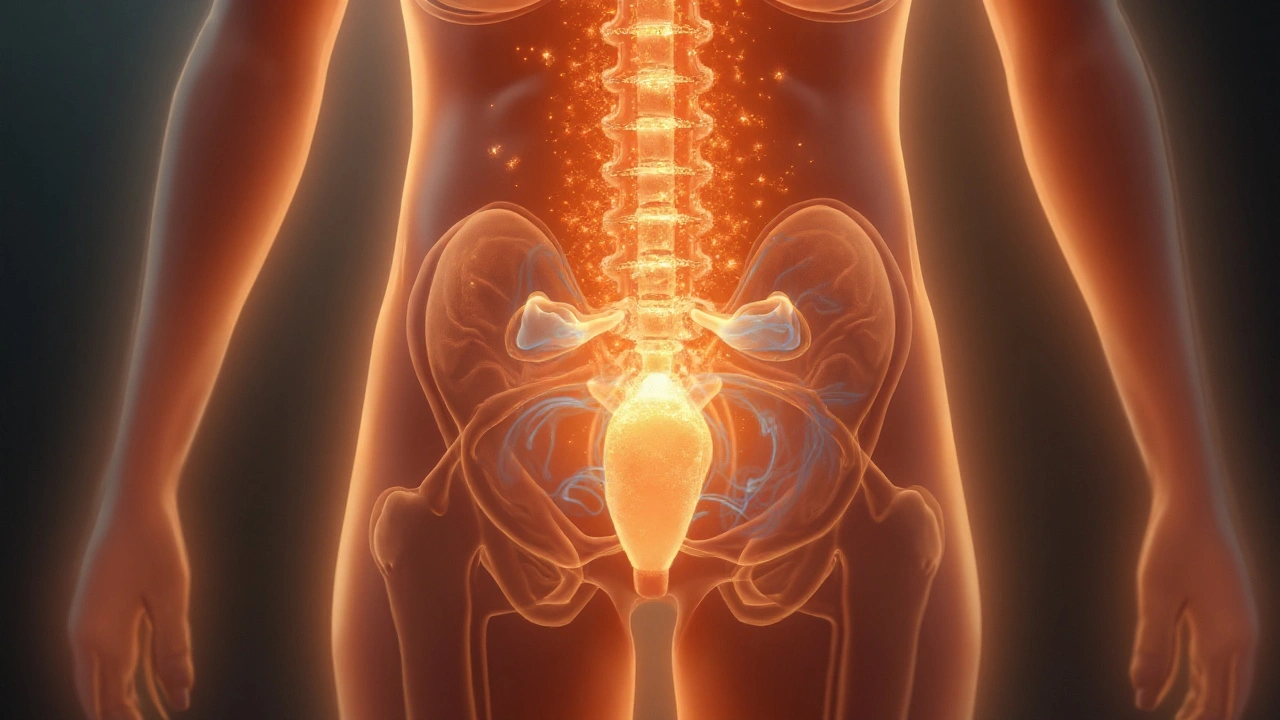
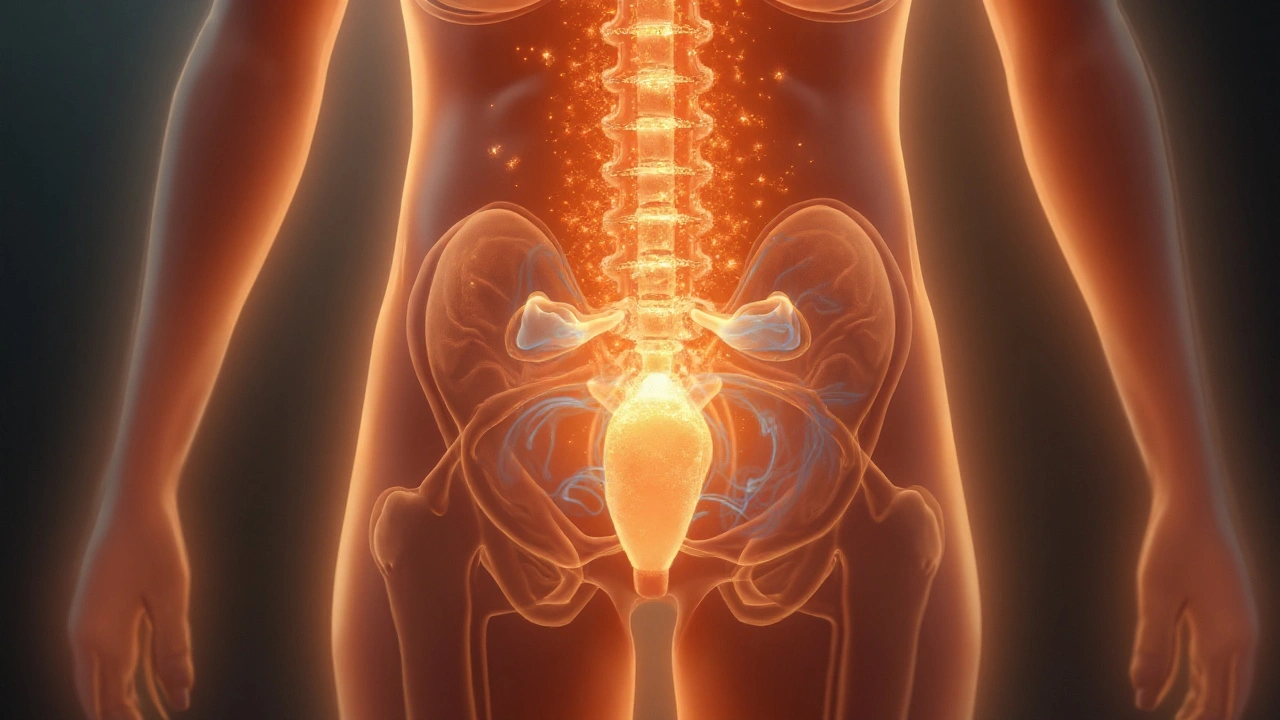
Understanding Bladder and Urinary Tract Muscle Spasms in Multiple Sclerosis
Explore why muscle spasms in the bladder and urinary tract happen in multiple sclerosis, how they’re diagnosed, and the most effective treatment options.
25 Sep 2025If you’ve ever heard the term “neurogenic bladder” and felt confused, you’re not alone. It simply means the nerves that tell your bladder when to fill and empty aren’t working right. When those nerves are damaged, the bladder can leak, hold too much urine, or refuse to empty at all. The result is uncomfortable and can affect daily life.
Common reasons for nerve damage include spinal cord injuries, multiple sclerosis, Parkinson’s disease, stroke, or even certain surgeries. Anything that interrupts the signal between the brain, spinal cord, and bladder can cause neurogenic bladder. Knowing the cause helps doctors choose the best treatment plan.
The bladder relies on a delicate balance of signals. If the nerves sending “full” messages are weak, you might feel urgency without any urine left. If the “empty” signals are missing, urine can build up and cause overflow. Both situations lead to symptoms like frequent leaks, sudden urges, dribbling, or a feeling that you can’t fully empty your bladder.
Doctors usually confirm neurogenic bladder with a few simple tests: a urine analysis, bladder ultrasound, and a urodynamic study that measures pressure and flow. These tests tell them whether the bladder is overactive, underactive, or both.
Managing neurogenic bladder starts with a solid routine. Try to empty your bladder on a schedule—every 2–4 hours—even if you don’t feel the urge. This helps prevent overflow and reduces the chance of infections.
Watch your fluid intake. Sip water throughout the day, but avoid gulping large amounts at once. Limit caffeine and alcohol because they can irritate the bladder and increase urgency.
If you need a catheter, clean the insertion site with mild soap and water each time. Use a fresh catheter as directed, and watch for redness, swelling, or foul-smelling urine—signs of infection that need immediate medical attention.
Medications can also help. Anticholinergic drugs calm an overactive bladder, while alpha‑blockers relax the neck of the bladder to improve emptying. Your doctor will decide which pills fit your situation.
Some people benefit from bladder training exercises, like pelvic floor muscle contractions (Kegels). These strengthen the muscles that support the bladder and can improve control over time.
In severe cases, surgery may be an option. Procedures such as bladder augmentation or a urinary diversion create new pathways for urine to leave the body safely.
Finally, keep track of what works and what doesn’t. A simple log of fluid intake, catheter changes, and any leaks can give your healthcare team clear data to fine‑tune your plan.
Living with neurogenic bladder can feel overwhelming, but a mix of routine, proper catheter care, medication, and occasional specialist input can make a big difference. Talk to your urologist about any new symptoms, and don’t hesitate to ask for help—your comfort and health are worth the effort.
Explore why muscle spasms in the bladder and urinary tract happen in multiple sclerosis, how they’re diagnosed, and the most effective treatment options.
25 Sep 2025