When you pick up a generic pill at the pharmacy, you expect it to work just like the brand-name version. But how do regulators know it will? The answer lies in something most people never hear about: dissolution profile comparison. This isn’t just lab jargon-it’s the invisible gatekeeper that decides whether a generic drug is safe, effective, and ready for your medicine cabinet.
What Is a Dissolution Profile, Really?
A dissolution profile is a graph that shows how quickly a drug dissolves in a liquid under controlled lab conditions. Think of it like timing how fast a sugar cube melts in water-but for pills. For a tablet to work, it must break down and release its active ingredient into your body. If it dissolves too slowly, you won’t get enough medicine. Too fast, and you might get too much too soon.
Regulators test this using machines called dissolution apparatuses. The most common one is USP Apparatus 2-the paddle method. It spins a metal paddle in a beaker of fluid that mimics your stomach or intestines. The fluid’s pH changes depending on the drug: pH 1.2 for the stomach, pH 6.8 for the small intestine. Temperature is held steady at 37°C, just like your body. Samples are taken every 5 to 30 minutes until at least 85% of the drug has dissolved.
They test 12 individual tablets or capsules from both the brand-name product and the generic. Not just one. Twelve. Why? Because real life isn’t perfect. One tablet might be slightly harder, another a bit softer. You need to see the whole pattern, not just a single result.
Why Compare Dissolution Profiles Instead of Doing Human Trials?
Imagine having to test every new generic drug on 50 or 100 people just to make sure it works. That’s expensive, slow, and ethically tricky. That’s where dissolution profile comparison comes in.
Since the 1990s, the FDA and other global agencies have accepted that if two drugs dissolve in nearly the same way under the same conditions, they’re likely to behave the same way in your body. This is called a biowaiver-a shortcut that skips the full human bioequivalence study.
According to FDA data from 2022-2023, 78% of generic drug applications used dissolution profile comparison to prove equivalence. For drugs classified as BCS Class I (highly soluble, highly permeable), this method is accepted in over 90% of cases. It cuts development costs by up to 60% and speeds up approval by 12 to 18 months. That’s not just efficiency-it’s access. More generics mean lower prices and more people getting the medicine they need.
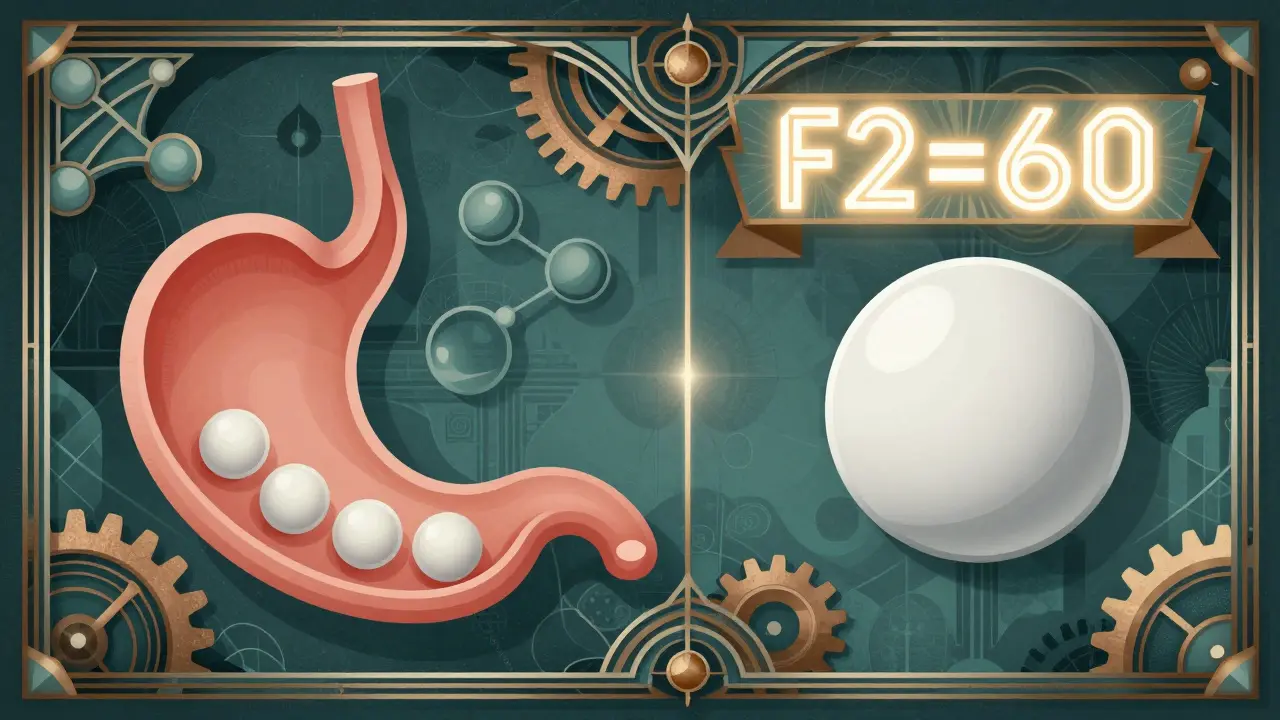
The f2 Similarity Factor: The Industry Standard
The most widely used tool to compare dissolution profiles is the f2 factor. Developed in 1996 by Moore and Flanner, it’s a mathematical formula that measures how similar two curves are.
The f2 value ranges from 0 to 100. A score of 100 means the two profiles are identical. A score between 50 and 100 is considered similar enough for regulatory approval. Anything below 50? That’s a red flag.
Here’s how it works: For each time point (say, 10, 20, 30, 45, and 60 minutes), the percentage dissolved for both the test and reference product is recorded. The formula calculates the average difference across all time points. Smaller differences = higher f2.
But here’s the catch: f2 isn’t magic. A 2021 University of Maryland study found that f2 can sometimes miss differences in how a drug releases-especially when the release mechanism is different. One tablet might dissolve fast at first but then slow down. Another might start slow but catch up later. Both could have the same f2 score, but your body might absorb them differently.
That’s why experts like Dr. Diane Bunick warn: “f2 methodology fails to account for the temporal sequence of dissolution.” Two profiles can look alike on paper but behave differently in real life.
When f2 Isn’t Enough: Advanced Methods
For tricky cases-like highly soluble drugs that dissolve too fast, or low-dose pills where tiny variations matter-f2 alone isn’t enough.
Here’s what regulators now recommend:
- Bootstrapping f2: Instead of one f2 number, you run the calculation 1,000 to 10,000 times with random samples to create a confidence interval. If the lower bound of that interval is still above 50, you’re good.
- Mahalanobis Distance Test (MDT): This method looks at the whole shape of the curve in multiple dimensions. It’s better at spotting differences in variability. A 2021 study showed MDT correctly identified dissimilar profiles in 94% of cases, compared to 82% for bootstrapped f2.
- AUC ratio: Area Under the Curve measures total drug released over time. Combining f2 ≥ 50 with an AUC ratio between 0.80 and 1.25 makes the prediction of bioequivalence 23% more accurate than f2 alone.
Some labs use model-dependent methods like Weibull or first-order models. These are more precise for complex release patterns but require more math and justification. The FDA doesn’t reject them-but they expect you to explain why you chose them.
What Makes a Dissolution Method Discriminatory?
Not all dissolution tests are created equal. A good method doesn’t just measure how much dissolves-it catches differences that matter.
For example, if you’re testing a generic version of a drug that’s been reformulated, your test must be able to spot if the new version dissolves slower due to a change in binder or coating. That’s called discriminatory power.
The FDA requires labs to prove their method can detect differences by testing stressed samples: tablets that were overheated, crushed, or stored too long. If your method can’t tell the difference between a normal tablet and a damaged one, it’s not good enough.
Real-world example: A Pfizer scientist on the AAPS forum said they once had a generic candidate with an f2 score of 49.8-just 0.2 points below the limit. The formulation was chemically identical to the brand. But because the tablet hardness varied slightly, the dissolution curve shifted. They had to redesign the entire formulation. The in vivo performance was unchanged, but the f2 failed. That’s how strict this system is.

Common Pitfalls and How to Avoid Them
Many generic manufacturers fail dissolution testing-not because their drug is bad, but because of sloppy testing.
- Apparatus misalignment: If the paddle isn’t centered or wobbles more than 1mm, the flow changes. That alters dissolution. A 2022 survey found 73% of failed comparisons were due to equipment issues, not product differences.
- Wrong media: Using just pH 6.8 for a drug that dissolves best in the stomach? You’ll miss critical differences. For BCS Class I drugs, you need tests at pH 1.2, 4.5, and 6.8.
- Insufficient volume: If the dissolution medium doesn’t have enough volume to keep the drug dissolved (sink condition), the drug will start to re-precipitate. That skews results.
- Skipping calibration: Temperature must be within ±0.3°C. Vessels must be concentric within 0.5mm. These aren’t suggestions-they’re FDA requirements.
Successful companies invest in training. The University of Maryland offers an 80-hour certified course in dissolution testing. Teams need 40-60 hours of hands-on time and 20 hours of stats training. Documentation is non-negotiable: every calibration log, every raw curve, every line of code used in analysis must be saved.
What’s Changing in 2026?
The rules are evolving. In 2023, the FDA proposed tiered f2 thresholds: f2 ≥ 65 for drugs with a narrow therapeutic index (like warfarin or lithium), and f2 ≥ 50 for others. Why? Because small differences in these drugs can cause serious side effects.
The EMA now requires confidence intervals around mean dissolution profiles at every time point-not just one f2 number. And biorelevant media? That’s the future. Instead of plain buffer solutions, labs are now using fluids that mimic real stomach and intestinal contents, including bile salts and enzymes. This is especially important for poorly soluble drugs (BCS Class II).
AI is also entering the scene. Thirty-seven percent of top pharmaceutical companies are testing machine learning models that predict how a dissolution profile will translate to human absorption. This could one day replace even the f2 test-but we’re not there yet.
What This Means for You
When you take a generic drug, you’re trusting that this invisible science worked. Dissolution profile comparison is the invisible handshake between regulators, manufacturers, and patients. It’s not perfect-but it’s the best tool we have to ensure generics are safe, effective, and affordable.
It’s why your $5 generic works just like the $50 brand. Not because they’re the same pill. But because scientists measured every drop, every minute, every variation-and made sure they matched.
What does an f2 score of 60 mean for a generic drug?
An f2 score of 60 means the dissolution profile of the generic drug is very similar to the brand-name version. It falls within the FDA’s acceptable range of 50-100, indicating the two products release their active ingredients at nearly the same rate under controlled conditions. This similarity strongly suggests the generic will perform the same way in your body, making it eligible for regulatory approval without needing human bioequivalence studies.
Why do some generics fail dissolution testing even if they’re chemically identical?
Even if two pills have the same active ingredient and dose, differences in inactive ingredients (like binders, coatings, or fillers) can change how fast the tablet breaks down. Manufacturing factors like tablet hardness, compression force, or granule size also affect dissolution. A generic might be chemically identical but physically different-leading to an f2 score below 50. That’s why regulators test the whole product, not just the chemistry.
Can a drug with an f2 score of 48 still be safe?
Regulators won’t approve it based on dissolution alone, but clinical studies have shown that some products with f2 scores between 48 and 50 still work the same in the body. The EMA’s 2017 review found 18% of such cases showed therapeutic equivalence. However, the f2 limit is a safety buffer. If a product fails f2, manufacturers must either reformulate or conduct full bioequivalence studies in humans to prove safety.
Do all generic drugs need dissolution profile comparisons?
Almost all immediate-release solid oral generics do. For modified-release products (like extended-release pills), it’s required. For some complex forms-like injectables, inhalers, or topical creams-other tests are used. But for tablets and capsules, dissolution profile comparison is the standard. In 2022, 95% of generic applications for immediate-release products included this data.
How long does it take to develop a valid dissolution method?
Developing a discriminatory dissolution method typically takes 8 to 12 weeks. This includes testing across multiple pH levels, varying agitation speeds, and stressing the product (like heating or aging tablets) to ensure the method can detect even small changes. It’s not a quick test-it’s a full validation process that must prove it’s sensitive enough to catch differences that matter.

This is why I don't trust generics. They're just cheap knockoffs pretending to be the real thing. Who even knows what's really in there? I'd rather pay extra and know I'm not risking my health.
lol i read all this and my brain just said 'so... if it dissolves like the brand, it works?'
yeah ok cool. i guess my $4 pill is fine then. thanks science.
in india we call this 'copy medicine' and it saves lives. my dad takes blood pressure pills that cost 10 rupees instead of 1000. no drama, just works. thank you science.
so america lets foreign labs test our drugs with paddle machines? that's ridiculous. we should be doing all this in-house. why are we trusting some guy in Bangalore to measure how fast a pill melts?
the dissolution profile comparison is a cornerstone of modern pharmacopeial science. it ensures therapeutic equivalence without unnecessary human trials. this methodology has been validated globally and remains indispensable for equitable drug access.
man, i used to work in a pharma lab and let me tell ya - the paddle ain't just spinning, it's got attitude. one time the temp was off by 0.5°C and we got f2 scores jumping like a kangaroo on espresso. calibration ain't optional, folks. it's the difference between 'works' and 'oops we gave grandma a heart attack'.
also, f2=60? that's like saying two songs sound similar even if one's in C major and the other's in C# - close enough for government work, but your ears might notice.
so if f2 is below 50, they have to test on people? that seems fair. i just hope they don't cut corners just to save time. medicine isn't something you wanna rush.
...so we're trusting math... to mimic biology... which is inherently chaotic... using a paddle... in a beaker... at 37°C... while ignoring the fact that human guts aren't lab beakers... and yet... somehow... it works??
is this science... or is this a beautiful, fragile, statistically significant illusion? 🤔🤯
also... f2=60... sounds like a lukewarm compliment from your mom after you cooked pasta. 'it's... fine.'
but hey - if it gets pills to the people? i'll take the illusion.