When standard antidepressants fail, what’s left? For nearly one in three people with depression, medications like SSRIs and SNRIs simply don’t work. That’s where ketamine and esketamine come in - two fast-acting options that can lift severe depression in hours, not weeks. Unlike traditional drugs that take months to show results, these treatments can turn things around after just one session. But they’re not the same. One is an IV infusion. The other is a nasal spray. One is off-label. The other is FDA-approved. And the differences matter - especially when your life is on the line.
How Ketamine and Esketamine Actually Work
Both drugs target the brain differently than older antidepressants. Instead of boosting serotonin or norepinephrine, they act on glutamate, the brain’s main excitatory chemical. This triggers a cascade of changes that rebuild damaged neural connections - something antidepressants rarely do. It’s not just about mood. It’s about repairing the brain’s wiring.
Ketamine is a racemic mixture - meaning it contains both the (R)- and (S)-forms of the molecule. Esketamine is just the (S)-form, purified and concentrated. That small chemical difference changes everything: how strong the effects are, how long they last, and how intense the side effects feel.
Think of it like this: ketamine is the full version. Esketamine is the streamlined one. Both get you to the same destination, but one takes a rougher road.
IV Ketamine: Faster, Stronger, But More Intense
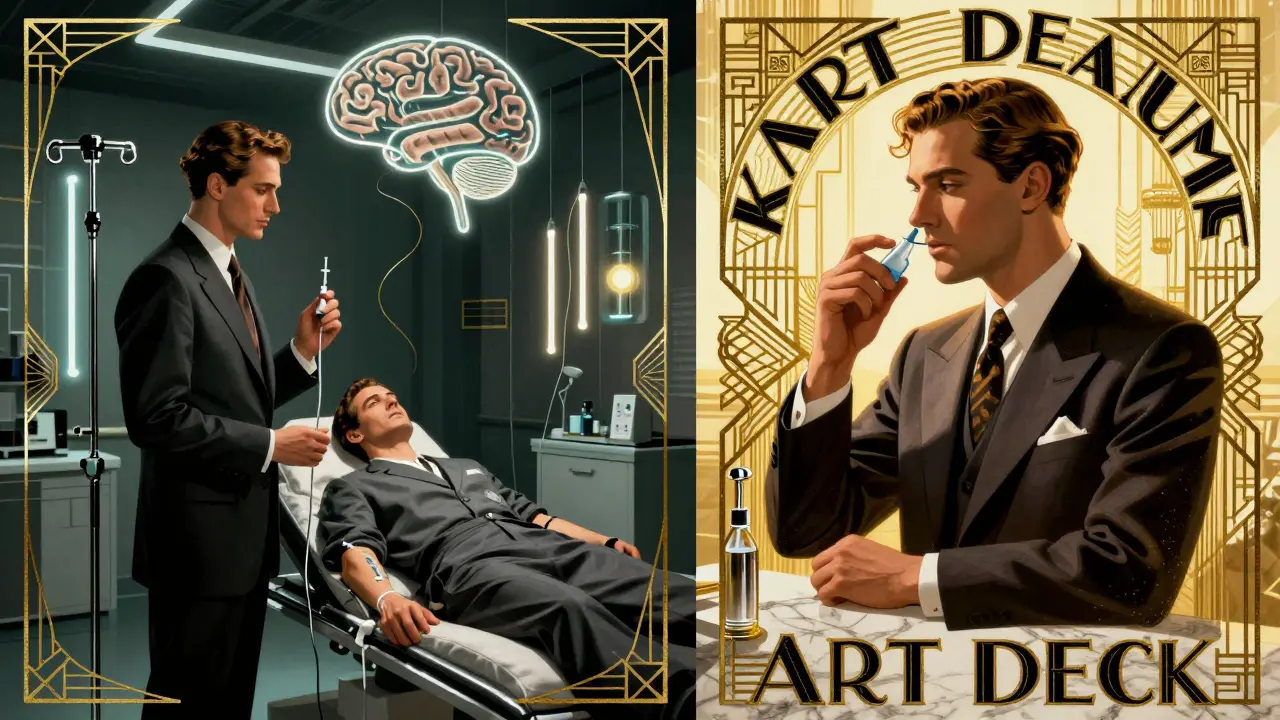
IV ketamine is given through a vein, usually over 40 minutes, at a dose of 0.5 mg per kilogram of body weight. Patients sit in a reclining chair, often with dim lights and calming music. Within minutes, they may feel detached from their body - a sensation called dissociation. Some describe it as floating. Others feel anxious. It’s not hallucinogenic in the psychedelic sense, but it’s definitely not normal.
That dissociation is the trade-off. In a 2025 study of 153 patients with treatment-resistant depression at McLean Hospital, those getting IV ketamine saw a 49.22% drop in depression scores after their final treatment. That’s more than half the symptoms gone. And it happened fast - improvement showed up after the very first dose.
But it’s not easy. About 42% of patients reported moderate to severe dissociation. Some needed extra monitoring. A few had nausea or increased blood pressure. Because of this, IV ketamine must be given in a medical setting with trained staff ready to handle complications. You can’t take it home. You can’t drive after. You have to stay for two hours after the infusion.
Esketamine (Spravato): Easier to Use, Slower to Kick In
Esketamine, sold as Spravato, is a nasal spray. You sit in a doctor’s office, spray it into each nostril, and wait. No IV needle. No nurse adjusting a drip. Just a simple, non-invasive delivery. The dose? 56 mg or 84 mg, twice a week for the first month.
The upside? Dissociation is less common - only 28.7% of patients report it, and it’s usually milder. That’s why many patients rate their experience higher overall, even if the relief comes slower. In the same 2025 study, esketamine users saw a 39.55% drop in symptoms - still meaningful, but noticeably less than IV ketamine.
And it takes longer to work. Most patients didn’t feel better until after their second or third dose. That’s a problem if you’re in crisis. But for people who need ongoing support, not emergency relief, the gentler ride makes sense.
Who Gets Which Treatment?
It’s not one-size-fits-all. If you’re actively suicidal or your depression is so severe you can’t get out of bed, IV ketamine is often the first choice. Its speed saves lives. Dr. John Krystal at Yale puts it plainly: “For life-threatening depression, IV ketamine is the clear winner.”
But if you’ve tried everything and just need a steady improvement - without the intense side effects - esketamine might be better. Dr. Christine Denny at Columbia notes that esketamine’s convenience makes it ideal for long-term use. You can go to your psychiatrist’s office, get your spray, and leave. No need for an anesthesiologist or IV setup.
There’s also a third group: people who can’t tolerate the dissociation at all. For them, neither option may be right. But for many, the trade-off is worth it.

Cost and Insurance: The Hidden Hurdle
Let’s talk money. A full course of eight IV ketamine infusions costs between $4,200 and $5,600. That’s out-of-pocket for most people - because only 38.2% of private insurers cover it. Even if your plan says it’s covered, many clinics won’t bill insurance directly, forcing you to pay upfront and fight for reimbursement.
Esketamine? It’s pricier - $5,800 to $6,900 for the same number of doses. But 67.4% of insurers cover it. Why? Because it’s FDA-approved. Insurance companies have rules. They pay for branded drugs with official labels. Ketamine doesn’t have that.
And here’s the kicker: even with insurance, you still pay for the clinic visit, the monitoring, the staff time. Some patients end up paying hundreds per session. That’s why access is so limited. Only 12.4% of U.S. counties have a certified Spravato center. Fewer still offer IV ketamine.
Long-Term Results and Maintenance
Neither drug is a cure. It’s maintenance. After the initial phase - usually 4 to 6 weeks - you move to maintenance dosing. For IV ketamine, that’s every 1 to 3 weeks. For esketamine, it’s once a week or every other week.
A 2024 study tracking patients for six months found that 56.3% of IV ketamine responders stayed in remission. For esketamine, it was 48.7%. That gap matters. The longer you stay well, the less likely you are to end up back in the hospital.
There’s also emerging science pointing to brain changes as predictors of success. A November 2025 study in Nature Mental Health found that patients who showed increased gamma wave activity in the frontoparietal region of their brain after the first dose were far more likely to respond long-term. This could one day let doctors test for response before starting treatment - no trial and error.
What About Safety?
Both drugs are Schedule III controlled substances. That means they have potential for abuse. But in a medical setting, that risk is low. Most patients don’t seek out repeated use outside of treatment. The dissociation isn’t pleasurable for most - it’s disorienting, sometimes frightening.
The real safety concerns are physical. Ketamine can raise blood pressure and heart rate. That’s why you’re monitored. People with uncontrolled hypertension, heart disease, or a history of psychosis are usually excluded. Esketamine has a slightly lower risk profile here, which is why it’s approved for use in more settings.
And while both require two hours of post-treatment monitoring, IV ketamine demands more: staff trained in advanced airway management. Esketamine only needs basic life support certification. That’s why you’ll find Spravato in more psychiatric offices than ketamine clinics.

The Future: What’s Next?
The field is moving fast. Janssen is testing a higher-dose version of Spravato - 112 mg - which could mean fewer treatments and better results. Meanwhile, researchers are testing intramuscular ketamine (injected into the muscle), which might offer a middle ground: faster than nasal, easier than IV.
And more clinics are popping up. In 2020, there were 142 ketamine centers in the U.S. By 2025, that number jumped to 1,087. More access means more people can try it. But quality varies. Not all clinics follow guidelines. Some push too many sessions. Others don’t screen properly.
That’s why it’s critical to choose a center with psychiatrists on staff, not just anesthetic technicians. This isn’t a spa treatment. It’s a medical intervention.
Real People, Real Results
On PatientsLikeMe, a mental health forum with over 1,200 users who’ve tried both, 63.2% of IV ketamine users said they felt relief within 24 hours. For esketamine, it was 51.7%. But when asked about their overall experience, 78.4% of esketamine users rated it “good” or “excellent.” Only 62.9% of IV ketamine users did.
Why? Because the nasal spray didn’t leave them feeling like they’d been knocked out. They could go back to work. They didn’t need someone to drive them home. The relief came slower, but the burden of treatment was lighter.
That’s the core tension: speed vs. comfort. Strength vs. sustainability.
Final Thoughts: Choosing Between Them
There’s no perfect answer. But there are smart choices.
If you’re in crisis - suicidal, unable to eat or sleep, stuck in bed - go for IV ketamine. The faster you get relief, the better your odds.
If you’ve tried everything and just need a steady lift, with less disruption to your life, esketamine is the way to go. It’s not as strong, but it’s easier to live with.
And if cost is a barrier? Ask about clinical trials. Many universities offer free treatment as part of research. Or look into payment plans. Some clinics offer sliding scales.
Either way, you’re not alone. And you don’t have to wait months to feel better. These treatments exist because people refused to accept that depression was a life sentence. They’re not magic. But for many, they’re the first real hope in years.
Is ketamine FDA-approved for depression?
Ketamine itself is not FDA-approved for depression - it was approved in 1970 as an anesthetic. However, its use for depression is off-label and supported by decades of research. Esketamine, the purified (S)-enantiomer of ketamine, is FDA-approved under the brand name Spravato® for treatment-resistant depression and depression with suicidal thoughts.
How quickly do ketamine and esketamine work?
IV ketamine often shows symptom improvement within hours - sometimes after the first dose. Esketamine typically takes two to three doses before noticeable relief. In a 2025 study, IV ketamine users saw improvement after the first treatment, while esketamine users needed at least two sessions to show significant change.
Which has fewer side effects: ketamine or esketamine?
Esketamine has fewer and milder dissociative side effects. In the same 2025 study, 42.3% of IV ketamine users reported moderate to severe dissociation, compared to 28.7% for esketamine. Esketamine also has a lower risk of hallucinations and blood pressure spikes, making it safer for outpatient settings.
Can I take ketamine or esketamine at home?
No. Both require medical supervision. IV ketamine must be given in a clinic with trained staff and monitoring equipment. Esketamine is administered as a nasal spray in a certified provider’s office, followed by a mandatory 2-hour observation period. Neither is approved for home use due to safety risks.
Is one more effective than the other?
Yes - IV ketamine is more effective. A 2025 study of 153 patients found IV ketamine reduced depression scores by 49.22%, while esketamine reduced them by 39.55%. Other studies confirm ketamine’s superior efficacy across multiple time points, from 24 hours to eight weeks after treatment.
How much does treatment cost?
A full course of eight IV ketamine infusions costs $4,200-$5,600 out-of-pocket. A comparable course of esketamine (Spravato) costs $5,800-$6,900. Insurance covers 67.4% of esketamine treatments but only 38.2% of IV ketamine. Many patients pay out-of-pocket or use payment plans.
Do these treatments cure depression?
No. Neither ketamine nor esketamine is a cure. They provide rapid relief but require ongoing maintenance dosing. About half of patients stay in remission for six months with regular treatments. Long-term use is still being studied, but most patients need ongoing sessions to maintain benefits.
Who shouldn’t use ketamine or esketamine?
People with uncontrolled high blood pressure, heart disease, a history of psychosis, or substance use disorders are usually excluded. Pregnant women and those with a history of bladder problems from ketamine use are also advised against it. Always get screened by a psychiatrist before starting treatment.