Antibiotic-Warfarin Interaction Checker
Check Antibiotic Safety
Risk Level:
Timing of Effects:
Action Recommendations:
Based on current medical guidelines. Always consult your healthcare provider.
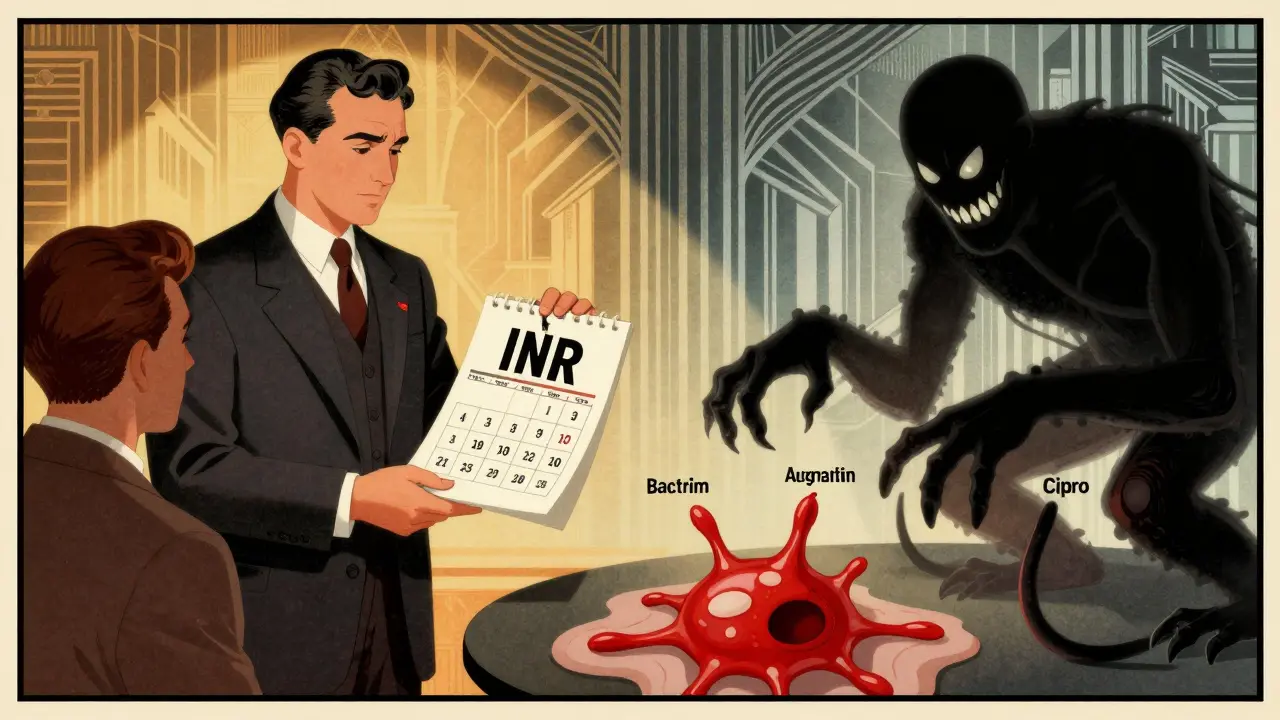
When you're on warfarin, even a simple antibiotic can throw your blood thinning off balance-sometimes with life-threatening results. You might think, "It's just a pill for an infection," but for people taking warfarin, certain antibiotics can cause INR levels to skyrocket in just a few days. And that means a much higher chance of serious bleeding: internal bleeding, brain hemorrhages, or uncontrolled bleeding from minor cuts. This isn't rare. In fact, antibiotics and warfarin interactions are one of the most common reasons older adults end up in the emergency room because of blood thinners.
Why Antibiotics Mess With Warfarin
Warfarin works by blocking vitamin K, which your body needs to make clotting factors. But your gut bacteria also make about 10-15% of your vitamin K. When you take antibiotics, especially broad-spectrum ones, they kill off those helpful bacteria. That means less vitamin K gets made, and warfarin ends up working harder than it should. Your INR climbs. And when INR goes above 4.0, your risk of major bleeding jumps 4 to 8 times. There’s another way antibiotics interfere. Some block the liver enzymes-CYP2C9, specifically-that break down warfarin. When those enzymes slow down, warfarin builds up in your blood. That’s why even if you’ve been stable on 5 mg a day for months, a course of ciprofloxacin can push your INR from 2.5 to 4.1 in under a week.Which Antibiotics Are Most Dangerous?
Not all antibiotics are created equal when it comes to warfarin. Some are high-risk. Others are safer. Knowing the difference can save your life.- High-risk antibiotics: Ciprofloxacin, levofloxacin (fluoroquinolones), erythromycin, sulfamethoxazole/trimethoprim (Bactrim), and amoxicillin/clavulanate. These can raise INR by 1.5 to 2.5 units on average. Ciprofloxacin alone increases bleeding risk by more than double.
- Medium-risk: Cefotetan and cefoperazone (some cephalosporins). These don’t affect liver enzymes but wipe out gut bacteria, causing delayed INR spikes-usually around day 5 to 7.
- Low-risk: Azithromycin, ceftriaxone, nitrofurantoin, and fosfomycin. These rarely cause INR changes. Azithromycin, for example, has almost no effect on warfarin metabolism.
- Opposite effect: Rifampin. This one doesn’t raise INR-it crashes it. It speeds up how fast your liver breaks down warfarin. If you’re on rifampin for TB or an infection, your INR can drop below 1.5, putting you at risk for clots and strokes.
A 2023 review found that 68% of warfarin-related ER visits involved just three antibiotics: ciprofloxacin, Bactrim, and amoxicillin/clavulanate. That’s not a coincidence. It’s a pattern.
When Does the Risk Happen-and How Long Does It Last?
Timing matters. The two mechanisms don’t hit at the same time.- CYP enzyme inhibition (like with ciprofloxacin): INR rises fast-within 2 to 3 days. It also drops fast once you stop the antibiotic, usually within 3 days.
- Gut flora disruption (like with Bactrim or amoxicillin/clavulanate): INR climbs slower. It often peaks between days 5 and 10. And here’s the kicker: it can stay high for up to 10 days after you finish the antibiotic. Many people stop checking their INR after the antibiotic ends. That’s when things go wrong.
One study of Medicare patients found the highest bleeding risk wasn’t during the first few days of antibiotics-it was between days 8 and 14. That’s when the gut flora effect kicks in hard, and people think they’re "out of the woods." They’re not.
What Should You Do? A Clear Action Plan
If you’re on warfarin and your doctor prescribes an antibiotic, don’t wait. Don’t assume it’s safe. Take action.- Ask your doctor: "Is this antibiotic safe with warfarin?" If they’re unsure, ask for a pharmacist consult. Pharmacists specialize in these interactions.
- Get your INR checked within 72 hours of starting the antibiotic. If it’s a high-risk one, check again in 3 to 5 days, and then weekly until 7 days after you finish the antibiotic.
- Don’t change your warfarin dose on your own. But do know this: for high-risk antibiotics like ciprofloxacin or Bactrim, many clinics reduce warfarin by 20-30% at the start of treatment. This isn’t guesswork-it’s standard practice at top anticoagulation clinics.
- Know the bleeding signs: Unexplained bruising, nosebleeds that won’t stop, red or dark urine, black or bloody stools, severe headaches, dizziness, or vomiting blood. If you notice any of these, call your doctor or go to the ER immediately.
- Keep a log: Write down your INR values, antibiotic names, and dates. Bring it to every appointment. It helps your provider spot trends.
Real-world data shows that when pharmacists manage warfarin during antibiotic use, bleeding complications drop by 37%. That’s not magic. That’s attention to detail.
What About Newer Antibiotics?
You might be prescribed something newer, like tedizolid (for skin infections) or linezolid. Good news: tedizolid has almost no effect on INR. Linezolid has a slight risk, but it’s much lower than ciprofloxacin.The 2024 review in Expert Opinion on Drug Metabolism & Toxicology confirmed what many clinicians suspected: even "safe" cephalosporins like ceftriaxone are low risk, but those with N-methylthiotetrazole side chains-like cefotetan-are dangerous. So don’t assume "cephalosporin" means safe. Always check the specific drug.

What’s Changing in the Future?
We’re moving beyond guesswork. Researchers are now using genetic testing to predict who’s most at risk. People with CYP2C9*2 or *3 gene variants break down warfarin slower to begin with. When they take an antibiotic, their INR can spike 2.4 times higher than others.The 2023 WARF-GEN trial showed that when patients were tested for these genes before starting antibiotics, and their warfarin dose was adjusted based on their genetics, INR instability dropped by 41%. This isn’t science fiction-it’s happening in specialized clinics now.
Electronic alerts in hospital systems help, but only if they’re smart. A 2019 study found that alerts alone reduced bad events by just 7%. But when they were tied to clinical decision support-like suggesting an INR check or dose adjustment-they cut events by 22%.
That’s the future: personalized, data-driven care-not one-size-fits-all advice.
Final Thought: You’re Not Overreacting
If you’ve ever been told, "It’s probably fine," when you were worried about an antibiotic and warfarin-you were right to question it. This isn’t a minor side effect. It’s a major, well-documented danger that kills people every year.The good news? You can prevent it. You don’t need to avoid antibiotics. You just need to be informed, proactive, and vigilant. Check your INR. Ask questions. Track your numbers. Speak up if something feels off.
Warfarin works. But it’s not a set-it-and-forget-it drug. Especially when antibiotics are involved. Your life depends on that small change in routine: checking your INR at the right time, and knowing when to act.
Can I take amoxicillin with warfarin?
Amoxicillin alone is low risk, but amoxicillin/clavulanate (Augmentin) can raise INR by about 1.2 units on average. This is because clavulanate disrupts gut bacteria that make vitamin K. Check your INR 3 to 5 days after starting it, and again 7 days after finishing. Don’t assume it’s safe just because it’s a "common" antibiotic.
How long should I monitor my INR after stopping an antibiotic?
For antibiotics that affect gut bacteria-like Bactrim, amoxicillin/clavulanate, or cefotetan-keep checking your INR for at least 7 to 10 days after you finish the course. The effect can linger. For CYP-inhibiting antibiotics like ciprofloxacin, 3 to 5 days after stopping is usually enough. But if your INR was high during treatment, keep monitoring until it’s back in range.
Is azithromycin safe with warfarin?
Yes, azithromycin is one of the safest antibiotics to use with warfarin. It doesn’t significantly inhibit liver enzymes or disrupt vitamin K-producing bacteria. Studies show only a 1.2-fold increase in bleeding risk-far lower than ciprofloxacin or Bactrim. It’s often the preferred choice when an antibiotic is needed for someone on warfarin.
Can I take over-the-counter painkillers with warfarin and antibiotics?
Avoid NSAIDs like ibuprofen or naproxen-they increase bleeding risk on their own. Acetaminophen (Tylenol) is generally safe at normal doses (up to 3,000 mg/day), but high doses can also affect INR. Always check with your provider before taking any OTC medicine, especially when you’re on antibiotics and warfarin. Two drugs that are safe alone can be dangerous together.
What if my INR is too high? Should I skip my warfarin dose?
Don’t skip doses on your own. If your INR is above 5.0, or if you’re bleeding, contact your anticoagulation clinic immediately. For INR between 4.0 and 5.0 without bleeding, they may advise holding one dose and rechecking in 24 to 48 hours. Never adjust your dose without professional guidance. Too much or too little warfarin can be deadly.
Do all antibiotics affect warfarin?
No. Nitrofurantoin and fosfomycin have little to no effect on INR. Azithromycin, ceftriaxone, and some newer antibiotics like tedizolid are also low risk. But the rule is: never assume. Always check the specific antibiotic. Even "low-risk" ones can interact differently in some people, especially older adults or those with liver or kidney issues.

lol so now i need a phd just to take an antibiotic? my grandma’s on warfarin and she thinks cipro is just a fancy cough syrup. she’s gonna die and it’ll be because someone wrote a 10-page essay on vitamin K.
I’ve been on warfarin for 8 years and this is the first time I’ve seen someone break it down this clearly. My pharmacist actually flagged amoxicillin/clavulanate for me last year-I didn’t even know clavulanate was the problem, not the amoxicillin. I started checking my INR every 3 days after starting antibiotics after that. No more ER trips. Seriously, if you’re on warfarin, find a good anticoagulation clinic. They’re not just for paperwork-they’re lifesavers.
Also, azithromycin is my go-to now. My doc switched me from cipro twice because I kept spiking. Azithro? Zero drama. I even told my sister to ask for it if she needs an antibiotic and she’s on blood thinners too. Simple, safe, effective.
And yes, track your numbers. I have a little notebook. I write the date, the med, the INR, and how I felt. It’s dumb, but when your INR hits 5.2 and you’re dizzy, you’ll be glad you did.
Also, don’t take ibuprofen. I learned that the hard way. One headache, two Advils, and I was bleeding from my gums for three days. Tylenol’s your friend. Always check with your pharmacist first. They’re the real MVPs.
And if someone says ‘it’s probably fine’? Walk out. You know better.
My dad almost bled out because he took Bactrim for a UTI and thought he was fine after 5 days. He didn’t check his INR after finishing. Ended up in the hospital with a GI bleed. This post saved my life. Seriously. I printed it out and gave it to my whole family. We all have someone on warfarin now. Thanks for this.
Also-azithromycin FTW. We use it for everything now. No more panic.
Antibiotic-induced INR elevation is a well-documented pharmacokinetic interaction primarily mediated through CYP2C9 inhibition and gut microbiota disruption, resulting in reduced vitamin K synthesis. The clinical significance is amplified in elderly populations with polypharmacy and reduced hepatic clearance. Proactive INR monitoring within 72 hours of initiation and continued surveillance for 7–10 days post-antibiotic discontinuation is evidence-based standard of care. Pharmacists should be integrated into anticoagulation management teams. Genetic testing for CYP2C9 variants further refines risk stratification. This is not anecdotal-it is clinical science.
Failure to implement these measures constitutes a breach of the duty of care.
Bro, I’m from India and my uncle is on warfarin for a mechanical valve. He took amoxicillin for a tooth infection and got scared. I showed him this post. He called his doctor, got azithromycin instead, checked his INR twice, and now he’s chill. 😊
Guys, this stuff is real. Don’t ignore it. A few extra checks can save a life. You’re not being paranoid-you’re being smart. ❤️
There’s an ontological crisis here, embedded in the very architecture of pharmaceutical intervention. Warfarin, as a molecule, is not merely a drug-it is a destabilizing agent in the homeostatic equilibrium of the human body. Antibiotics, as ecological disruptors, collapse the symbiotic microbial ecosystems that contribute to vitamin K homeostasis. The INR becomes a metric of fragility, a quantifiable index of vulnerability in a biomedical system that refuses to acknowledge its own fragility.
And yet, we reduce this to a checklist. ‘Check INR.’ ‘Ask your pharmacist.’ As if epistemological clarity can be purchased with a flowchart. The real danger isn’t the drug interaction-it’s the normalization of precariousness. We are taught to manage risk, not to question why our bodies require such constant surveillance. Why must we be so afraid of a pill? Because the system demands it.
But perhaps the answer isn’t better monitoring. Perhaps it’s better medicine. Warfarin is a 1940s solution to a 21st-century problem. We need alternatives. We need to stop treating coagulation like a dial setting.
And yet… I still check my INR. Because the system is all we have.
LOL this is why I switched to Xa inhibitors. Warfarin is a relic. Who still uses it? Grandmas and people who hate convenience. 🤡
Also, ‘check your INR’? Nah. I just take Eliquis and eat whatever I want. No more ‘gut flora this’ or ‘CYP2C9 that’. Just swallow a pill and forget it. The future is here, folks. Stop living in the 1950s.
Also, ‘azithromycin is safe’? Tell that to the guy who got torsades from it. 😏
Okay but what if you’re on warfarin AND you’re vegan? Do your gut bacteria still make vitamin K? Or do you need to take supplements? I’ve been reading about this and now I’m terrified. What if I’ve been quietly bleeding internally for months because I don’t eat eggs? Are we all just one antibiotic away from a hemorrhage?
Also, why is no one talking about the fact that probiotics might help? I took Culturelle after my last course of antibiotics and my INR didn’t spike. Coincidence? Or science? Someone test this. I’m not joking.
And why does the post say ‘don’t change your dose’ but then say ‘many clinics reduce it by 20-30%’? That’s not consistent. That’s just confusing. I’m not even on warfarin and I’m confused. What’s the right answer?
Also, who wrote this? It feels like a pharmaceutical ad disguised as a public service announcement. I smell a grant.
so like… if you take cipro and warfarin you can bleed out? wow. i thought it was just a cold pill. my cousin did that and he’s fine. maybe he just got lucky. anyway, i’m gonna take amoxicillin next time i’m sick. what’s the worst that could happen? 🤷♂️
The human body, in its biological complexity, is not a machine to be calibrated, but a dynamic system perpetually negotiating equilibrium. Warfarin, as an anticoagulant, does not merely inhibit vitamin K epoxide reductase-it imposes a metaphysical burden upon the organism, forcing it to live in a state of precarious balance, where even microbial life becomes a variable in the calculus of survival.
The antibiotic, in its indiscriminate destruction of gut flora, does not merely reduce vitamin K synthesis-it reveals the profound interdependence between human and microbial existence. We are not solitary entities, but ecosystems. To treat the body as a closed system is to misunderstand life itself.
And yet, we reduce this to a checklist: ‘Check INR.’ ‘Avoid Bactrim.’ ‘Use azithromycin.’ These are not solutions. They are adaptations to a flawed paradigm. The real question is not how to manage the interaction-but whether we should be prescribing warfarin at all in an age of direct oral anticoagulants.
Perhaps the most dangerous antibiotic is not ciprofloxacin, but complacency. The belief that medicine can be reduced to protocols, when in truth, it demands humility in the face of biological mystery.
And so, we monitor. We adjust. We survive. But we must ask: at what cost to our dignity? To our trust in the body’s own wisdom?